Access denied?
Socioeconomic inequalities in digital health services
18 September 2023
Reading time: 92 minutes
Executive summary
The UK’s health and social care system increasingly relies on digital services and the flow of patient data to deliver care to tens of millions of people. Digital transformation is intended to fuel innovation and efficiency and improve patient experience.[1][2] However, there is a risk that digital healthcare can exacerbate existing health inequalities.
For people involved in commissioning, developing and deploying digital health services, it is important to identify practical ways to mitigate inequalities and ensure the benefits of this technology are felt by all. Failing to do so can prevent people from accessing the care they need and widen health gaps between those who are able and those who are unable – for a variety of reasons – to use these services effectively.
Over the last three years, the Ada Lovelace Institute, in partnership with the Health Foundation, has explored how the accelerated adoption of data-driven systems and digital health services interact with health inequalities in the UK.
Data-driven health systems is the term we use to refer to technologies that collect, process, and analyse data about people to present health information in new ways, make predictions, or reach a particular outcome. They include risk prediction algorithms and population health dashboards like the COVID-19 Data Dashboard.[3] Data-driven health systems enable the sharing or dissemination of health data to a range of actors on the ‘backend,’ including data analysts and healthcare providers who use that information to deliver individual care or inform wider public health policy.
These systems may also include patient-facing digital health services, which seek to provide health information, advice, and care through digital tools like apps or online platforms. Both have been increasingly implemented as a result of the COVID-19 pandemic and the NHS digital strategy .
Effective digital transformation in the NHS requires digital services to be designed and developed with a deep understanding of how this technology will be experienced by patients, particularly those experiencing health inequalities.
In this report, we sought to understand how people who have lived experience of poverty and ongoing health concerns are impacted by health inequalities when interacting with patient-facing digital health services.
Using a participatory research method, we trained six people who have experience of poverty to become ‘peer researchers,’. They conducted 26 interviews with others in their communities across England and Scotland about access to digital health services, attitudes towards health data use, and health inequalities. Our collaborative approach to ethnographic research included knowledge sharing, co-production of research questions, and the peer researchers themselves conducting the fieldwork interviews with participants.
Using this method meant we could collaborate on research design with the peer researchers and engage deeply with people’s everyday experiences through interviews. In this way, our study uncovers some of the hidden ways that people experiencing poverty and chronic health concerns interact with digital health services – and amplifies voices that aren’t often heard in discussions around healthcare policy.
This report is not intended to provide a broadly representative picture of health inequalities in the UK, but in combination with other qualitative studies in different communities, can help in understanding the nuances of intersecting inequalities.
See ‘Methodology section’ for more detail.
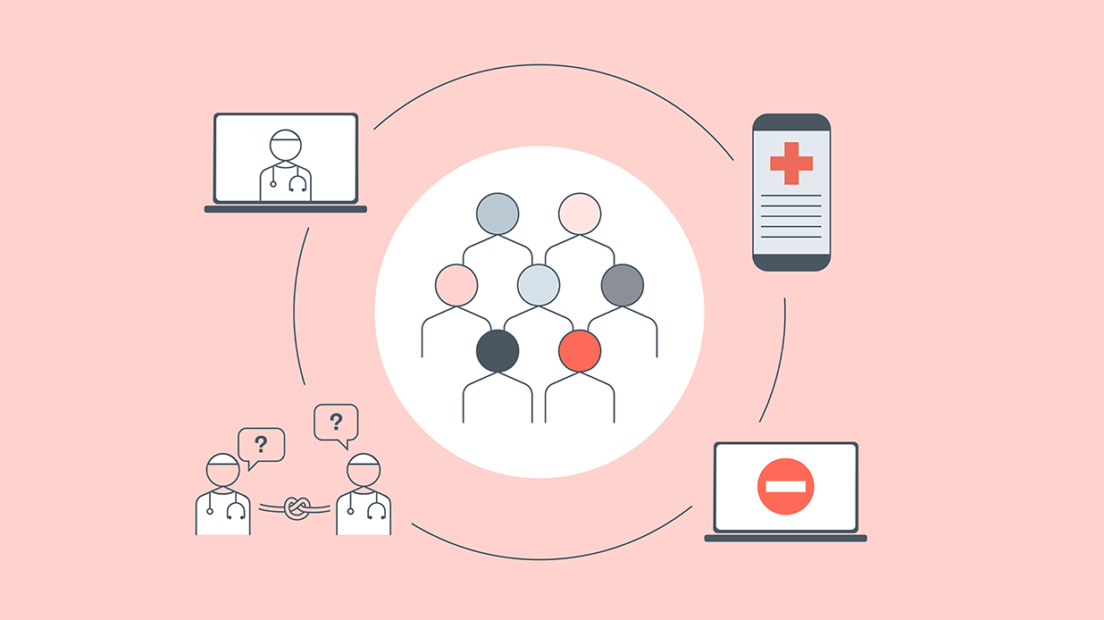
Our previous report, A knotted pipeline,[4] described how the UK’s health and social care system relies on a pipeline of data sourcing, sharing, and curation between government departments, local authorities, clinicians, public health officials and private sector organisations to make healthcare decisions. That report identified six ‘knots’ in the pipeline that cause and exacerbate health inequalities, including a lack of consistent data on inequalities and a diffusion of responsibility to address them systematically.
As a companion to A knotted pipeline, this report highlights the apparent difference in perspective between those working with data to plan healthcare interventions and design digital health services and those interacting with digital health services as patients. It exposes a misalignment between priorities for policy and industry regarding digital health services and what economically disadvantaged people (often with chronic or complex health issues) need and want from healthcare. This is a gap that needs to be bridged if healthcare policy and practice in the UK is to deliver benefits for everyone.
Our findings suggest that people who are responsible for designing, developing, and deploying digital health services should be encouraged and incentivised to better engage with and respond to different viewpoints throughout that process.
This report begins the work of unravelling a ‘knot’ that underpins the UK’s health and care system – that throughout the process of designing and deploying data-driven health systems, inequalities are poorly understood, described and measured. In doing so, this report provides an important perspective on other ‘knots’ concerned with the value of social context in datasets and the limits of how well data can represent lived experience. Broadly, our study makes the below findings:
- Digital health services are being designed and implemented without consideration of lived experience for some groups, particularly for those who are ‘digitally excluded.’[5] Our participants had concerns about not being consulted or informed about new digital health services. The inflexibility of many digital health services (like not seeing a suitable option on an online form or triage service, or not being able to use online platforms due to time, skills or cost constraints) is widening the health gap for some people with complex care needs or who experience poverty.
- Digital health services are making some people’s experience of healthcare less personal – people we spoke to value the doctor–patient relationship but feel like it is being eroded. Many of our participants felt like new digital health services were creating barriers to access and communication with clinicians (for example, through remote appointments or online triage systems).
- Health data isn’t working well for some groups experiencing socioeconomic disadvantages – our participants feel like it is not being used in the best way or seen by the right people. This is a tension: on one hand, there is scepticism about how the NHS handles sensitive data and who gets access to it, but on the other hand, people feel that medical professionals should be able to access the data when required, to save patients explaining themselves again at each new appointment. Both of these frustrations may be widely experienced but can hit harder for people who have multiple health conditions, are under stress due to socioeconomic disadvantage, or who feel stigmatised in interactions with the health system.
- Context matters for the development of digital healthcare – people are acutely aware of the crisis that the NHS faces, and it is being felt when they access (or have trouble accessing) healthcare. For many this manifested both in their routine interactions with the healthcare system (like booking appointments) and in perceptions of new digital health services (that they may be cost-cutting or efficiency initiatives over efforts to improve patient care). This situation can exacerbate inequalities through perpetuating a ‘digital divide,’ in which many people lack access or capability to use digital technologies,[6] and a ‘digital postcode lottery’ in which some localities lack the resources and infrastructure for patients or clinicians to use digital health services.
- Access to and experience of digital health services is shaped by the constraints or opportunities that exist at a local level – building regional capacity for the use of health data and increasing digital connectivity between patients and providers is good in theory but can risk benefitting some areas while others are left behind.
These findings highlight the need for policymakers, healthcare leaders, and digital health service designers and developers to reconsider how they use data and how they design and deploy digital health services.
According to the peer researchers and participants in this study, the success of these services may depend on factors that cannot be solved by technology alone: including how well resourced and supported the UK’s health and social care system is, how much people feel they can trust that system, and how well the system responds in a joined-up way to the needs of those experiencing inequalities. Addressing these challenges requires broader changes in the NHS, including workforce recruitment, retention and training, as well as the adoption of data governance practices that earn and maintain public trust in data sharing.[7]
Personal experience of socioeconomic inequalities, ongoing and complex health concerns, and differing levels of local health support inform what participants in our study want from their health service: a personal relationship with their doctor that isn’t entirely mediated by a digital platform; a reliable way for health professionals they trust to access their data; and the use of digital healthcare options that reduce admin burden and work for a range of complex needs – which may change over time. Overall, our research participants felt that (with some positive exceptions) this isn’t being achieved.
While our findings will not be applicable to everyone, the implications of this study are indicative of how digital health services can perpetuate or alleviate inequalities, providing a compelling call for further lived experienced research in this area. We hope these findings will be of use to people working on digital health services in the private and public sphere who want to learn more about how their products are experienced by people dealing with socioeconomic inequalities.
For policymakers and health officials especially, our findings suggest questions to ask and groups to engage with when developing policy or commissioning digital health services. For the developers or designers of these services, our findings demonstrate the importance of understanding often-marginalised perspectives to ensure digital health services are more inclusive and flexible.
We encourage others interested in inclusive technologies in society to build on our evidence and iterate it through engagement with those experiencing inequalities.
Place-based research
In a flat near Glasgow city centre, one interviewee talks about how their community is quite tight-knit, willing to help each other out in a bind. In a different part of Glasgow, an interviewee laments how hard it is to avoid hassle when walking around the local area but says the church group they’re in – which supports recovery from addiction – has been invaluable.
In Newcastle-under-Lyme, an interviewee worries about her asthma in a damp flat provided by a housing association; a bit further east, someone talks about how nice it is to be able to reach green space with a short walk.
A researcher living in Stoke describes the local healthcare provision as ‘pot luck,’ while someone living in Wiltshire is considering a move because there’s no healthcare support and the aqua-rehabilitation classes she was doing were moved too far for her to travel. Meanwhile, someone in Bristol feels lucky that her local GP is one of the best in the city.
This research is rooted in place: the perspectives and stories shared in interviews are situated in communities, and deeply connected to where people socialise, work, rest, and live.
The specificity of these experiences and the way they’re shaped by locality and community show us how inequalities might manifest in the routine and mundane – which is often overlooked and invisible from the outside. It shows that ‘marginalisation’ can look different for many people, and that geography still has an impact in the digital age.
Short audio clips of peer researchers discussing their local areas and communities
🔊Listen to a short audio clip of peer researchers discussing their local areas
Transcript
Peer researcher 1: To be fair, where I live isn’t my community because I don’t really engage with anybody where I live, really. I’d say hello to them, or what have you, you know, exchange Christmas cards, but it’s limited. People tend to keep themselves to themselves, especially when you know that five or six doors across the road, you’ve got a coke dealer who sells this, that, and the other, you tend to want to keep yourself to yourself. So my community is more Expert Citizens, and the friends I’ve made being involved with them.
Peer researcher 2: I live in an area in Glasgow called Possilpark. It’s highly deprived, high alcohol abuse levels, high drug levels. During the 80s and the 90s, it was kind of the drug centre of Scotland. But it’s no worse or better than anywhere else nowadays. But even though it’s got its problems, I wouldn’t want to live anywhere else. There’s a strong community there. And the community really works together, especially where children are involved. The children are the heart of the community. We’ve all come from similar backgrounds. None of us are particularly rich. We’re all kind of struggling from day to day. But saying that, the community does pull together when it’s needed, and it’s like anywhere up and down in the country, where you know your neighbours, and you look after each other. We’ve all got a responsibility to each other.
🔊Listen to a short audio clip of peer researchers discussing their communities
Transcript:
Peer researcher 3: I live in Glasgow, and it is a deprived area where I live. I mean, it’s a great community, very close-knit. Everybody knows everybody. We have a lot of social things and there’s food pantries, there’s parks, there’s children’s grow-your-own. You know, it’s quite an upcoming area, it’s being regenerated. But there is an awful lot of deprivation.
Peer researcher 4: Stoke on Trent? Well, everyone calls it ‘the potteries.’ Yeah, you know, ‘potbanks.’ It’s not a rich area in one sense of money and stuff. Most of the main streets are derelict, loads of the main shops, like, closed down and all the small businesses have disappeared. But Stoke-on-Trent is very rich in another way. We are lucky to have so much countryside surrounding Stoke-on-Trent. It’s like, in the communities I run in with work, it’s very uplifting, very much a community. But when you walk the streets, it’s a total different thing. We have lost our community side in Stoke-on-Trent, I would say. I remember when I was kid, there was, like, street parties and stuff like that. I think it’s become more individual. Technology hasn’t really helped. It’s kind of like dragged communities apart. Everyone’s still stuck on their phones walking the streets and stuff, or listening to music, or whatever, when really, we should be sharing all these experiences with each other.
A note on quotes
Throughout this report, any text in quotation marks represents quotes drawn from the transcripts of the peer researchers’ interviews.
Some quotes have been edited to improve readability, for example by removing repetition or filler words used as people articulated their thoughts. There have been no additions, word replacements or other edits that would change the meaning or sentiment of interviewees’ statements.
All interviewees are anonymous and we have assigned a letter to represent each interviewee.
Glossary of terms
Digital health services provide health information, advice and care through patient-facing digital tools. These tools include: apps used to make GP appointments and order prescriptions; remote appointment platforms; health tracking apps; online forms; and portals used to access electronic personal health records. In short, what patients see and interact with.
Data-driven health systems are technologies that collect, process, and analyse data about people to present health information in new ways, make predictions, or reach a particular outcome, (including data dashboards and diagnostics tools). The term includes the people who develop, design and deploy these technologies (including engineers, product teams, clinicians, hospital administration staff and others) and the insights they produce. This term refers more to the ways that data is used ‘behind the scenes’ and how it shapes the technologies that patients see.
Health and social care system refers to the collection of organisations that provide health and social care support to people, including GP practices, hospitals, dentists, and care homes.
Integrated Care Systems (ICSs) in England are partnerships of organisations in a particular area that come together to plan and deliver joined up NHS services.
Health boards and health trusts are regional bodies providing NHS services in Scotland, Wales and Northern Ireland.
Introduction
The acceleration of data-driven health systems and digital health services during the pandemic has reshaped people’s experience of care, and reframed the landscape in which health interventions are designed and deployed.
The NHS is rattling toward a digital future in pursuit of efficiency and innovation – with a trial of AI-driven technology to predict missed appointments underway, and a large new federated data platform (which would support data linkage across the NHS) in development.[8] It has expressed a keenness to develop the NHS App and online channels into a ‘digital front door’ to ‘give patients access to quicker and more effective care at their fingertips and save the health and care system time and money.’[9]
There is a strong focus on AI and data for preventative care, digitisation to increase clinician productivity, and equipping individuals to access data about their own health online.[10] This is accompanied by the much more rapid proliferation of AI and data-driven health technologies in the private sector, including personalised healthcare programmes like ZOE[11] and remote monitoring tools like MySense AI.[12]
The continued push to implement digital health services in the NHS and private sphere comes at a time of multiple crises in the UK around the cost of living, energy, and employment – the pressures of which are being felt unequally.
These crises are impacting people’s lives from all directions, fuelling societal inequalities and highlighting the importance of social determinants in health. Healthcare providers have raised the alarm about the effect fuel poverty will have on health inequalities[13] and during a cost of living crisis, data poverty may force more people offline and reduce their access to essential health services.[14]
Citizens Advice research from May 2023 shows that one million people cancelled their broadband in the preceding year due to cost pressures, with people receiving Universal Credit more than six times as likely to have disconnected compared to people not receiving Universal Credit.[15]
At the same time, the NHS faces its own challenges around funding and costs that are driving the digitisation of the health service: there is a keenness from health officials to harness technology for ‘efficiency, economic growth, and private investment,’[16] as well as using the NHS App to help with issues of access to care[17] and the use of AI diagnostics to free up clinicians’ time.[18]
Increased NHS efficiency is a worthy goal and digitisation is a key part of that mission. But it is important to ask: who feels the benefit of this acceleration of digital healthcare, and who gets left behind, or locked out? And how will a future NHS that centres digitisation and data retain the high levels of patients trust, human relationships and lived experience that are so core to the health service? [19]
Against this backdrop, our research seeks to understand how well digital transformation is playing out for a group of people experiencing socioeconomic disadvantage: are digital health services currently offering better care for these patients? And what is the impact of social context on how well digital healthcare works for them?
The Ada Lovelace Institute and the Health Foundation have been working in partnership to explore how the accelerated adoption of data-driven health systems like population health dashboards and digital health services like GP-access apps during the pandemic may have affected inequalities, and the ramifications of this for the future of healthcare. The aims of the partnership are set out below:
- To develop the evidence-base around the interaction between data-driven health systems, digital health services and health inequalities
- To build a shared understanding of what action is needed to reduce inequalities in health and improve health outcomes
- To encourage prioritisation of health inequalities in the design of policy and in the development and use of data-driven systems and digital health services.
The first output of the partnership, in 2021, was The data divide, a public attitudes survey that highlighted causes of inequalities that come not only from health datasets, but from the ability to participate in digital healthcare.[20]
In that report, we found that digital health services have not been experienced equally, and that this divide – between people who do and people who do not access digital healthcare – has a knock-on effect for who is considered in the design and development of future technologies and the future of healthcare in general. Barriers to access were more likely to be experienced by the most clinically vulnerable people and those on the lowest household incomes (less than £20,000 per annum).
In November 2022, we published a landscape review, A knotted pipeline, which, through desk research and interviews, described the complex interplay between data-driven systems and health inequalities in the UK’s health and social care system.[21]
It contended that the data pipeline is complex, messy and full of pinch points (‘knots’) that contribute to downstream inequalities, and emphasised the need for a people-centred approach to data-driven health systems. This means all actors involved in the development and deployment of these systems must take responsibility for addressing health inequalities.
For example, commissioners should require that data to monitor inequalities is part of the technology they commission; data analysts working with health data should bring an understanding of social context into their decisions; and product designers or engineers should demonstrate how they have considered inequalities in design and testing.
The participatory research that underpins this report picks up on the public attitudes seed planted by The data divide and the findings of A knotted pipeline, and further explores the intersection of digital healthcare and inequalities at a case study level. We see this paper as an important piece of the puzzle – asking how digital health services affect the everyday experiences of and access to healthcare for a group of people experiencing socioeconomic inequalities.
It deviates from A knotted pipeline perspective to show the situation from another side: where that report gathered perspectives from those working to commission, design, and deploy digital health services, this report involved speaking to people experiencing those services on the other end of the process.
For this part of the project, we sought to answer four questions:
- How do social contexts and conditions interact with health inequalities in relation to digital health services?
- How does the use of health data to develop digital health services impact on social inequalities?
- How does the advancement of digital health services affect the everyday experiences of and access to healthcare?
- How could a human-centred approach inform the way users are seen and designed for in digital health services?
We took an ethnographically-informed participatory approach – variably called PEER ethnography (Participatory Ethnographic Evaluation and Research),[22] collaborative ethnography[23] or community-based participatory research (CBPR)[24] – and provided support and training for six community members from across England and Scotland as peer researchers.[25]
We wanted to get a regional spread of perspectives to see how local and social contexts and conditions shaped everyday experiences of digital health services and inequalities
As the peer researchers conducted the interviews in their own communities, they already had the trust and shared context with community members needed to gather nuanced insights in a safe and relaxed environment for the participants.
The value of this approach has been demonstrated in other recent research. This includes the British Red Cross’s Offline and Isolated report,[26] which uses peer research to look at how digital exclusion impacts people seeking asylum, and ClearView’s Diverse Voices on Data report for Understanding Patient Data,[27] which examines the views and experiences of people from Black and South Asian communities in the UK on how their health data is collected and used, partially through peer-led research. Lived experience and public engagement work is also ongoing across many parts of the NHS and research institutions through patient and public involvement and engagement.[28] [29]
This method meant that we could learn from the lived experience expertise of our peer researchers in collaborative research design. In co-designing interview questions with the peer researchers, we heard that digital health services impacted their lives most, especially GP-access and health tracking apps, e-consult forms, online prescription platforms and getting text updates from the doctor.
The researchers were also interested in personal data collection and sharing and linking. This led us to focus on patient-facing digital health services and personal health records for this report. In A knotted pipeline, we focused more on data-driven health systems like population health dashboards and risk-prediction algorithms, which people don’t necessarily interact with directly, but which do have an impact on their lives.[30]
🔊Listen to a short audio clip of peer researchers discussing the research questions
Transcript:
Peer researcher 4: I would say coming up with the questions themselves – that stuck in my mind, because we were all sat around the table in the Grand Hotel eating rhubarb and custard shortbread. Yeah, that way we came up with the questions, that was the most interesting thing. We were basically writing all the things we could think about, about the data of healthcare, where it’s being used, and we were putting it all into categories.
Peer researcher 2: I think that this is a value of peer research. We’ve been involved in all the stages. If I remember right, one of the point I added was that the original questions used far too much technological language, and that can put distance between the questioner and the person who has given up their time to answer the questions. And it’s the expertise of the peer researchers that changed that.
Peer researcher 3: I thought the hardest bit was actually breaking it down in the smallest amount of questions, but to cover everything, but I mean, it was quite good because a lot of them did interact. It was trying to get all this interaction into one question.
The key findings of this report span three overarching themes:
- Access to digital healthcare
- Health data and data sharing
- The broader UK healthcare context.
It became clear in our findings that there is a gap between the expectations of how digital health services will serve patients and how they are being experienced by some groups in reality. For example, people reported not having the mobile data or credit to access remote appointments or health information online; being sent back and forth by an e-consult form that doesn’t have the right options; and generally feeling like digital health services and health data sharing initiatives were being pushed through with a ‘one size fits all’ approach that did not fit them.
This report offers insight and evidence from people who find that digital health services do not work well for them, and whose perspectives are often marginalised. It suggests ways of gathering more evidence that digital health service developers and designers, policymakers, and commissioners should use to better design services for those with complex health and care needs. In each section of the report, we summarise the implications of our findings. These are related to the everyday lives of the people that participated in our study.
An understanding of how these systems are experienced by marginalised groups can help improve services for those who might otherwise be overlooked. This leads us closer to a human-centred approach to the design and deployment of digital health services.
This study is based on a small group and aims to examine the specificities of their lived experience. It is not intended to be representative of the many intersecting experiences of health inequalities, and a particular limitation is that there is little ethnic diversity among the group. This work contributes to a body of evidence on digital healthcare and inequalities in the UK, and can be built on by further research in collaboration with different communities.
How to read this report
…if you’re a policymaker or commissioner concerned with digital health services or data-driven health systems:
- The findings offer insight from people with lived experience of socioeconomic health inequalities that are important to consider in planning and implementing digital health services.
- The implications under ‘How health data is used’ show why communication and trust is important for the success of using patient data, and using lived experience to understand limitations in clinical data could result in better tailored interventions.
- The implications under ‘Seeing digital health services as part of a broader context’ show that public perspectives towards a struggling health service (for example, scepticism about new digital health services as cost-cutting measures, or as barriers to access) must be taken into account when planning new digital health services.
- Under the same section, policymakers and commissioners should consider the way that postcode lotteries may be replicated in the digital context: for example, if different regions have different capacity for digital transformation in the health service, the benefits of this will be felt unevenly.
…if you’re a developer or designer of digital health services or data-driven health systems, or a healthcare practitioner using them:
- The findings show the often-invisible ways that digital health services have the unintended impact of exacerbating health inequalities. These emphasise, along with the introduction, the importance of engaging these perspectives, which often differ significantly from those working within data-driven systems.
- The implications under the section, ‘Access to digital healthcare’, suggest further considerations that could be made in development to ensure digital health services are more inclusive and flexible for differing needs of patients.
- The implications under the second section, ‘How health data is used’, are a reminder of the importance of looking for ways that lived experience might differ from what is presented in data, and to flexibly respond to that information.
- The implications under the second section, ‘How health data is used’, make the case for why public trust in data sharing must be earned to enable data sharing projects to be successful.
… if you’re a researcher or public engagement practitioner interested in technology and society:
- The ‘Methodology section’ describes what we did in detail, as well as how and why, which may also offer insight for others interested in undertaking similar participatory research methods.
- The findings help build up a bank of evidence from marginalised voices, which provides an insight into how some communities interact with digital health services, and how digital health services impact health inequalities.
Findings
An analysis of the interviews that the peer researchers conducted revealed findings along three broad themes:
- Access to digital healthcare: participants found digital health services could make access to care more difficult and create a barrier to communication with health professionals.
- How health data is used: participants reported concerns about fragmented data records and data that was not representative of their lived experience.
- Seeing digital health services as part of a broader context: participants routinely cited wider concerns around the NHS, including underfunding, workforce strain and the perceived incursion of private organisations in the health service as a reason for scepticism about new digital health services or data sharing projects. This theme also covers regional variation in digital workforce skills and resources, which could mean some areas benefit from digital transformation while others are left behind.
Access to digital healthcare
🔊Listen to a short audio clip of peer researchers discussing access to digital healthcare
Transcript
Peer researcher 3: There is the health centre, but if you’re fit enough, you can walk. But, if you haven’t got the bus fare to get there, a lot of people just won’t go because you can’t afford two pounds for two bus stops. And, like for all the COVID jabs, so you have to go to the mosque, so that’s like 15 pounds in a taxi each way. So people just won’t go. Why can’t they have it in the doctors’ like used to have with the flu jabs. People could always get nearer to a health centre to get it, but they won’t pay money, so that’s only going to have a bigger impact on the NHS. Very few people, I would say, do have access to computers and that. And the few that do, they said they’ve even tried to get onto an NHS website and do things, but they can’t get on, or they don’t understand it. And a lot of people don’t trust it. And they wouldn’t know how to navigate – they say it’s too hard to navigate. People just don’t trust digital. A lot of people don’t have computers, and a lot of people don’t know how to use it.
Digital health services, such as apps for remote care, can offer accessibility for those who are confident with digital options and can reduce admin burden for simpler tasks like repeat prescriptions.
‘I’d much rather do things via phone or video, simply because if you’re working full time you don’t have to physically come to the GP surgery, right? You can just do it over the phone, wherever you are. If I’m at work I can just take 20 minutes out from work and just have the call or whatever it is and talk to them. It saves both of us a lot of hassle and time and travel.’ – Interviewee A
‘So it’s a repeat prescription, and I order that through the Patient Access system, so I never have to clog up my doctor’s time, I don’t have to ring the surgery, I don’t have to go in there, I simply go online, order the damn stuff, say I’ll pick it up from the pharmacy, which I think they’ve grasped that’s what I want to do, and it’s just there.’ – Interviewee B
But this is not the case for everyone or at all times. Currently, digital health services are being implemented without consideration of lived experience for people who are socioeconomically disadvantaged and are not addressing structural issues in the health service – like access to care.
From the very start of working with the peer researchers, the broader topic of digital healthcare kept coming back to this key issue of not being able to get an appointment or communicate properly with a healthcare professional (including GPs, specialists, and mental healthcare providers). The feeling amongst peer researchers was that digital health services are either not addressing this, or actively exacerbating the situation.
Many interview participants – especially those with a higher health burden, complex needs, or who may be ‘digitally excluded’– felt that digital health services are making care less personal, and they missed having an ongoing relationship with a clinician who knows them and their history.
‘I think they’re already becoming far too reliant on telephone conversations, consultations and Zoom things, and yes, that’s not healthcare. That’s a very good buffer to see maybe who needs to come in sometimes but this isn’t healthcare.’ – Interviewee D
Many participants also felt that remote appointments could compromise the quality of care they received, worrying that there was a digital barrier that would prevent important cues and contextual information from being picked up. There were a couple of examples where people felt they had been misdiagnosed due to having to communicate their symptoms through video calls or pictures sent via text.
‘In one scenario I can remember, J’s doctor, he had an issue with skin, these things on his hands, and they actually asked me to take pictures of it and send it to them on WhatsApp. And I’m like, ‘What? Why do you just not want to see him?’ And it was, ‘Oh, we can deal with it this way … but she misdiagnosed his hands through the pictures, but you could just tell it wasn’t scabies, because I was touching his hands and I wasn’t getting it’ – Interviewee E
‘So, really good doctoring is to do with knowledge of the patient, knowledge of the patient’s background which is very important … and knowledge of where they live because if you live in a damp and horrible house, which I’m lucky enough not to, then that’s going to impact terribly on your health. If you live in a very polluted city, which I do, that’s going to impact on your health as well. All these things are so important and they’re all lost through the digital age. So, I deplore it.’ – Interviewee C
This suggests that developers and designers of digital health services like remote care platforms or health tracking apps should consider how they could facilitate rather than replace human interaction, for those who want that continuity and a personal relationship in care.
These concerns were also related to a feeling of not having a say in how digital transformation is changing healthcare. Our participants still wanted to be able to trust in the NHS to look after them and have their best interests at heart, but many felt like digital health services were being pushed through over their heads, with little agency or consultation in the matter.
‘I think it would be very useful if there could be a timely communication from all centres to patients about various apps because so many of us have smartphones.’ – Interviewee B
‘Just don’t get me started on that thing [the contact tracing app]. It was snuck on my phone, without my permission, well the basis for it was. And before you ask me how that made me feel, it made me feel irate … yes, that was next level bullshit, as far as I’m concerned.’ – Interviewee F
Many GP surgeries use the NHS App or third-party apps like Patient Access, myGP and Klinik to book appointments, order repeat prescriptions or share medical records. But when signing up, there’s often multiple options for patients to choose from, little guidance on the functional difference between them, and a lack of understanding about who has control over the data collected and stored within.
‘Probably the biggest downfall of digital technology is the lack of sharing of information to help with understanding the systems in the first place, you know, and the uses it’s used for. And like you said before, where’s all this information go? Now, that should be something to let people know before you even sign up to anything.’ – Interviewee G
According to our participants, the introduction of digital health services (like the NHS App) needs to come along with good information, transparency and communication from national and local health bodies, otherwise important trust in the health service is lost. For those who aren’t so comfortable with digital options, there’s a question of whether there’s an actual choice to opt in or out, or if it’s ‘just the way it’s done now’[31] without accompanying advice and reassurance about how they work.
This is particularly salient in the aftermath of pandemic lockdowns: when reflecting on our initial findings in a January 2023 workshop, one of the peer researchers observed that a lot of this seemed to have been rushed through in an emergency situation, and that policymakers never thought to re-assess how it was all working for a range of patients when the dust had settled.
It is worth noting again that for some people the NHS App and other apps enabling GP access offer valuable convenience. We heard examples from people who had mobility issues, anxiety about going to the GP in person, and an appreciation of having their medical information stored on their phone who were positive about using these apps. But we also heard in some interviews that people were confused about the functionality of the NHS App, and that this was sometimes patchy.
‘I think the NHS App is quite straightforward, just personally speaking, and I think generally as well it’s quite a straightforward app. The only issue with the app was that it said you couldn’t make appointments for a while on it, you couldn’t get advice from your GP – and that’s one of the main reasons why I was using it. So it was just saying unavailable. But obviously I’ve just checked there and you can book appointments and stuff again now.’ – Interviewee O
‘Basically, getting registered on it was a right nightmare because it just wouldn’t accept any of my information at first. I got registered on it and then it just wouldn’t accept anything. It was like my banking app, but what got me about my banking app was I could physically go into the bank and go, ‘Why isn’t this working? Tell me why.’ The manager solved it in two minutes. It’s like, why is there not an equivalent for the NHS?’ – Interviewee J
With the NHS App at the heart of the digital health strategy,[32] engaging with marginalised groups on why they use or don’t use it, and what is or isn’t working for them is vital. This could also include ways to feedback through the system so that when users experience issues that can be flagged within it, that information can be used to update or improve the system.
Overall, there were concerns around digital exclusion and how this could drive unequal access to healthcare, particularly for those on low incomes who can’t afford to pay for phone data or broadband, older people who struggle with technology,[33] or homeless people who can’t register for digital health services if they have no fixed address or photo identification.
In our digital-first world, we can now see digital determinants of health interacting with and complicating the traditional social determinants of health. For example, access to healthcare services as a determinant of health now is also affected by accessibility and usability of telehealth platforms; housing as a determinant of health now may also include lower access to decent broadband in more deprived areas.[34]
In evaluating Government commitments made on digitisation of the NHS in England, an expert panel appointed by the Health and Social Care Select Committee asserted that ‘the groups experiencing health inequalities are often those most at risk of digital exclusion,’ and that there is a risk that the health of digitally excluded groups will decline further as health and social care provision becomes increasingly reliant on access to and comfort with using technology. It found that successful delivery of digital health and social care was hampered by insufficient planning to mitigate this digital exclusion.[35]
As a recent Kings Fund report on digital exclusion in health and care pointed out, ‘in reality, it is possible for anyone to be digitally excluded at some point as their health or personal circumstances change.’[36] It was a current lived reality for many of our interview participants.
‘Smartphones always cost extra money and then you’ve got to buy the data every month, and it’s not every month, myself, I have the money to purchase my data.’ – Interviewee Q
‘You can’t just walk in anymore, and say, ‘Can I make an appointment for such, and such a date?’ They say, ‘No, you have to go away, and ring up?’ Now, if somebody hasn’t got credit, or even access to a phone, or anything like that, what are they supposed to do? This sounds like I’m a real anti-digitalist doesn’t it? But I’m not, because it has got its uses. It makes everything so much more accessible, I just think it’s being used in the wrong way.’ – Interviewee G
‘It’s all computerised. So, you know, I think with my age group, because, you know, I didn’t grow up with new technology, I’ve been struggling to learn what I have learned so far, pretty much on my own. So I still make mistakes on my phone and, you know, I still need computer support.’ – Interviewee H
‘And there’s no person-centred involvement, really, anymore, whatsoever. It’s very digitalised, and people such as myself, I hate technology, and if I can’t, like, phone up, and speak to a person, like a receptionist, or something like that, then I tend not to bother’ – Interviewee G
Even if people are able and willing to use the tech, digital health services are often inflexible for people with complex needs or experience of multiple disadvantages, so an overreliance on them in the provision of healthcare could still widen health gaps. If a digital health service is too ‘one size fits all,’ or when the complexity of people’s lives isn’t legible in the data it uses, this is likely to have a disproportionate impact on people affected by multiple disadvantages.
‘The systems themselves are quite exclusionary, you know, because I work with people with experiences of multiple disadvantages and they’ve been heavily, heavily excluded because they say they have complex needs, but what it is, is that the system is unwilling to flex to provide what those people need to access those services appropriately.’ – Interviewee I
‘It’s all right ticking boxes [but] sometimes you don’t feel that box is you, although it says ‘other.’ Other is just a word, it doesn’t mean anything.’ – Interviewee S
For some of our participants, having to navigate digital health services made existing access issues (like long waiting times) worse by as patients felt even further from having someone to talk to or knowing the right pathway to take.
‘One of the services that they have at the surgery is called e-consult whereby you get a form and you’re asked questions about the condition that’s troubling you. I did that twice when I had a problem … and at the end of it, on each occasion it said, ‘we can’t help you, you need to see a doctor’ – it just tells you to see a doctor and it’s because you can’t get to see a doctor that you did the e-consult in the first place. It’s a vicious circle.’ – Interviewee C
‘So they brought in this app thing that they encourage you to go straight to. And of course I’ve tried it and it was far too crude. It didn’t cover anything much, except for very basic things and it wasn’t going to answer the questions that I had or help me in any way, and they’ve limited everything, really, all sorts of access.’ – Interviewee H
These findings show that while digital health services may make some people’s lives easier, they can also add complicating layers and decisions to already time-consuming tasks like getting a GP appointment – particularly for those who don’t have reliable internet access or digital skills. Even seemingly small barriers to healthcare, like frustration with tech, can cause people not to seek healthcare in a timely way.
These barriers can lead to unequal health outcomes by disproportionately impacting those who are already under pressure. In the case of our participants, many felt less able to navigate these platforms due to constraints with having multiple jobs, caring responsibilities or limited data allowance, or health concerns like ongoing fatigue, chronic pain and neurological symptoms. In many cases, these issues intersected with digital exclusion and a feeling of a lack of agency in the healthcare system.
Digitisation may make the NHS more ‘streamlined’ or ‘efficient’ on the surface, but this doesn’t translate to better care for everyone; ‘efficiency’ can end up being good for some and not others. Designing for use-cases that reduce friction for people who don’t have a lot of time, have a higher health burden, or who have limited technical proficiency could help with this.
One participant talked about a general acceptance of some people experiencing worse health than others. This wasn’t specifically about digital healthcare, but it really resonates when read within that context, when exclusionary systems are adopted and little support is given to those left out.
‘I do think marginalised communities suffer more than most. I mean, obviously working in the field that I do, LGBT, obviously the AIDS crisis and things, LGBT people suffered because it was just not known and not accessed. Because it wasn’t seen as affecting the populous, it was seen as affecting a small group of people. Similarly, I think that’s how disability’s seen in a lot of circles. It’s like, ‘Well, of course you’re going to have these issues. You’re disabled.’ – Interviewee J
Something that the researchers and interviewees emphasised was that there should always be a non-digital option for people who need it or if things go wrong. Part of the role of those designing digital health services is knowing where digital doesn’t fit, and as mentioned before, trying to retain pathways for human interaction.
‘We must never solely rely on that because there are people … of my age and older who will not get to grips with it at all. I do think that, even if we digitalise health, how we access it, how we record it, how we ask for advice, how we get results, and so on, I do think that a human element should be digitalised completely out because you know, we’re human and we thrive on contact.’ – Interviewee B
Implications
- Currently, many digital health services are being implemented without consideration for the complexity of lived experience, and in particular, the needs of those with higher health burdens. Choice and flexibility of digital and non-digital care pathways based on patient preference and circumstance is needed. Engagement with patients who have complex health needs or might be digitally excluded, ideally through trusted community groups,[37] would help healthcare providers and those designing or deploying digital health services understand their needs.
- With the NHS App as one of the key parts of NHS digital transformation, it is important for developers to understand – and continuously ask as functionality evolves – what patients (especially those who experience health inequalities or who are at risk of digital exclusion) are finding helpful and not helpful about it, who isn’t using it and why.
- It is imperative to design digital health services in a way that facilitates, and doesn’t replace, the doctor–patient relationship. This could start with commissioners and healthcare providers ensuring patient choice and information over their digital and non-digital care pathways.
- Those working to develop digital health services could focus on interventions like automation for more straightforward admin and operational tasks, in ways that free up clinicians’ time with patients to maintain continuity for those who want it.
- Digital exclusion can drive health inequalities, and vice versa: consideration needs to be made of those who have limited access to digital health services or are less comfortable using them. Initiatives to make digital health more inclusive include local authorities or ICSs and health boards providing devices, data plans, and digital literacy training to those experiencing socioeconomic inequalities.
- It is unclear how free a choice people have to opt in or out of using digital health services, and if they’ve just been adopted by default in a post-lockdown world: commissioners and developers of these services should consider taking a step back to communicate use-cases for these tools and figure out whether they’re always appropriate, through qualitative and quantitative evaluation.
How health data is used
🔊Listen to a short audio clip of peer researchers discussing how data is used
Transcript:
Peer researcher 4: Data is like a collective of information. It’s information about people, information about the things that they’ve done, or not done. I suppose data is one of the most important things in this generation, really. Because it can tell you about everything that every person does – each individual person. And it’s a very expensive commodity at the moment. It’s very important that we protect it.
Peer researcher 2: In a personal sense, it’s the history of your life so far, it can be a useful tool to have on someone, but it can also be used and misused. Especially now as been proven through various votes and things where data was used to focus information being targeted at people, not always for a good thing. And it can be increasingly weaponized as well.
Peer researcher 3: Data is a lot of statistical figures. But there isn’t enough qualitative data, especially around lived experiences. And that’s what you need – the true reality of lived experiences to inform data. People will read that more and listen to it more than looking at a set of figures
In the delivery of health and social care services, healthcare providers, researchers, charities, and NHS partners collect, store and use a variety of data about a patient’s health. It can span across different clinics, providers, and types of care, and consists of details taken at GP registration and consultations, hospital appointments and prescriptions issued.
For many people we spoke to, there is a scepticism about how health data is being used: our participants overwhelmingly feel like it is not being used in the best way or seen by the right people.
There is a real tension between a desire to better join up personal health data so clinicians get a good idea of what the patient is going through, and resisting over-datafication of patients or relying only on clinical data to understand someone’s situation.
Our participants reported that what health data says about someone often doesn’t reflect lived reality and can be devoid of important nuance. This echoes a couple of key findings in our A knotted pipeline report – that data always has its limits as a proxy for truth and reality, and that data read without historical and cultural context might be misleading.[38] Confusing or inaccurate data can be harder to manage for people who have less time or agency to advocate for themselves in a healthcare setting, and who might feel stigmatised or misunderstood in this setting.
‘I feel like it’s really unhelpful to be constantly reminded that I’m overweight and almost diabetic, but there not be any follow-up support for that … It’s like, ‘This is a ‘you’ problem, so go and fix it. Okay, see you.’ Whereas what they don’t see, because it’s not on my records because I never went through services for my addiction. So what they don’t see is that I put all of this weight on because I was so busy focusing on trying to stay clean that I let other stuff go.’ – Interviewee I
‘There was a health check, a national health check that was done, for example […] some of the metrics for it, and measurements for it, […] hadn’t been done correctly at all. It was like sort of, glossed over, tick-the-box exercise rather than helpful for the person.’ – Interviewee B
For developers and deployers of digital health services, this presents an opportunity to think about the other ways that people’s health needs can be understood when planning healthcare interventions, and the importance of having a holistic approach, relying not just on clinical data but looking for ways to create networks of multidisciplinary knowledge in healthcare.
Strengthening relationships between primary care and voluntary and community sector organisations could help combine insights that clinicians get from health data with contextual knowledge from charity organisations, and community/patient groups about the type of support that different groups might need. Social prescribing is an important part of this – connecting people with non-clinical community-based support for wellbeing. This includes referrals to things like swimming classes or advice on housing and welfare, targeting key determinants of health that aren’t represented in clinical data.[39]
When it came to clinical data, we also found that fragmented records can adversely affect people’s experience with healthcare. On a personal care level, participants reported that poor use of data adds a burden of having to explain themselves over and over when seeing different medical professionals.
This is something that many people can relate to, but it can have a higher impact on people who are experiencing multiple disadvantages, multiple or ongoing health conditions, or for whom recounting their health issues in this way is traumatic.
‘Having the information in different places is ridiculous if you’ve got more than one healthcare professional trying to access that data. With services that we’re working with, they have issues when clients have got multiple disadvantages, like, things like mental health issues alongside addiction, and so they are having to repeat their stories over and over, and over again, and sometimes re-traumatising themselves.’ – Interviewee F
This suggests that for some people, the data they have already provided (in the form of GP notes and prescription records, for example) could be better used and shared between medical professionals. However, the collection of more detailed data about people in a centralised location raises other kinds of risks around privacy and surveillance that could further derail trust in healthcare for many people who already have good reason to be wary.[40] Some of our research participants expressed a concern, for example, that people deciding on their benefits or insurance payments might have access to their health data.
A recent report by the Institute for Government (IfG) on data sharing during the pandemic highlighted the importance of public trust in the success of data sharing projects. It used the General Practice Data for Planning and Research (GPDPR) patient data sharing scheme as an example, where a lack of public consultation and meaningfully seeking consent from patients led to millions of people opting out and the scheme being put on hold.[41]
In a private roundtable that was held as part of the IfG research, recommendations based on lessons from GPDPR included showing rather than telling the public how a data project works and what the benefits are, and providing more detailed information for patients on how their data is being and has been used, as well as information about redress for any breaches.[42] Ideas like this resonated with our peer researchers when mentioned in a workshop in January 2023.
It was clear throughout the interviews that people don’t understand how their data is being used or protected by health and care professionals. Participants said they didn’t know who exactly has access to their health data, and whether partnerships between the NHS and private companies affect the security of that data.[43]
‘I think these tech companies, these software designers, see the health service coming and I think they just see it as a big money bag. And actually, you probably could develop this stuff a lot cheaper, and a lot better than the billions of pounds that the health service paid for some of this kit, and some of this technology.’ – Interviewee M
‘I’m not sure that all of the information is kept just to making services better within the NHS. I think it’s used for [corporations] and large companies that do not have the patients’ best interests at heart, I don’t think. And I think this, because I know that the NHS being split up into 42 different boards, and each of those boards has a place on it for private enterprises.’ – Interviewee F
‘I’ve heard so many stories and you don’t know what’s misinformation, and what’s true. I’m concerned that it can be shared with the DWP without my permission. I’m concerned that it could be shared with other organisations.’ – Interviewee T
People aren’t against data sharing to improve population health, but they want to be informed about how this is happening. There are always going to be differing levels of engagement with this, but the information should be accessible and available for those who want it.
‘I think we all have to be just a little careful and make sure as services change that, you know, making sure that the public are on board about how things are working, and making sure that [data controllers are] not misusing data, let’s say, or sharing without agreements and so on. I think sharing health information with no patient identifiable data is useful because it allows services to get a flavour of the public’s health in general, but it has to be non-identifiable information.’ –Interviewee N
‘I don’t think it’s right that all and sundry should have access to it [medical records]. That should be specific. That should be very specific, definitely.’ – Interviewee R
Implications
- Commissioners, researchers, data analysts and healthcare providers using clinical data to plan healthcare interventions should make sure to acknowledge the limitations of quantitative data, and actively look for ways that lived experience might differ. This is another argument for technology not replacing the important doctor-patient relationship: on a direct care level, having a doctor with some contextual knowledge of the patient would help.
- Fragmented data can worsen the patient experience. This is particularly bad for those in traumatic situations or who – like many in our research – feel stigmatised in a medical situation and have less time and agency to navigate the system. If this issue is connected to interoperability of data systems as well as time-poor clinicians not being able to read notes, it could be another area where improvement of IT systems and automation of admin and operational tasks would be helpful.
- Better understanding is needed about why some people mistrust health data sharing and how that trust can be built up meaningfully – with the onus being on data users and controllers like the NHS and any private partners to build trustworthy systems. Initiatives to tackle this mistrust could include mandating public engagement and advisory groups of citizens and subject experts around data sharing projects in the public sector, as suggested by the IfG,[44] and continuing work on platform security with Trusted Research Environments for analysis of NHS data.[45]
- There is a delicate balance between improving patient experience through better data linkage and maintaining patient confidentiality: this is a live issue and one that requires further research and attention.
Seeing digital health services as part of a broader context
🔊Listen to a short audio clip of peer researchers discussing digital health service
Transcript:
Peer researcher 1: Health care in my area is rubbish. I moved doctors’ [surgery] because my doctors’ [surgery] was rubbish, that was close to me, and moved to one further away, and for a while, it was better. However, then, then it just seemed to follow suit of everybody else. And you have to be available all day for an appointment and phone up at eight o’clock in the morning. So they’ve now refused to take prescriptions over the phone. So you’ve either got to do that through a third-party app, which I’m very aware is mining your data. Or you can phone up the chemist, if they’ll answer the phone. The few and far between ones that were reasonable seem to be going down that slidey slope to conform with everybody else.
People we spoke to are acutely aware of the crisis that the NHS faces, and it is being felt when they access (or have trouble accessing) healthcare. For many of our research participants, it has discouraged them from seeking care at all. A lot of interviewees felt that COVID-19 had made the situation worse – partly through the accelerated adoption of digital health services – but most were careful to assert that the healthcare crisis pre-dated the pandemic.
‘I just think the whole systems are appalling at the moment and have been since lockdown. I know it was like this beforehand, but it’s just gotten worse. It’s gotten worse.’ – Interviewee C
‘I don’t think [healthcare] is as tailored as it can be, because of, I guess, the lack of NHS staff and funding, and all that type of thing, I don’t think GPs, or not GPs necessarily but the people in that field have all of the time and resources to take in all the information, be able to properly diagnose, get you the right information, get you the right services.’ – Interviewee O
Digital health services operate within the wider context of the UK health and social care landscape: this context shapes the way that people experience the benefits or drawbacks of digital healthcare and data sharing discussed in the sections above.
The issue of NHS funding and resource drain was an important topic to a lot of the peer researchers and interviewees: concern about the state of the NHS and the political machinations behind this came up in nearly every conversation and was an unmissable piece of the puzzle when discussing health inequalities. This highlights that digital health services must be designed and deployed with the specific constraints of the social and political landscape in mind.
Developers and commissioners of these systems must consider how their systems will be perceived at a time when the health of the UK population is declining[46] and healthcare workers are striking on an unprecedented scale over poor pay and benefits.[47]
A concern raised by other research is that a lack of time and resources in the health service could be wrongfully seen as a problem that technology alone can address, and fuel ‘techno solutionism.’[48] This is not to say that smart use of digital health services and data-driven health systems won’t be part of addressing challenges for healthcare in the UK, but that issues around digital exclusion and health data sharing will be exacerbated if digital health services and data-driven health systems are rushed in to paper over cracks in the NHS.
This poses a risk to patient trust: public perceptions and experiences of an underfunded, understaffed NHS can mean efforts to digitise health services are seen as cost-cutting first and foremost, rather than efforts to improve care.
As this report suggests, engaging with members of the public, and especially marginalised groups, must inform the way that digital transformation in the health and care system is rolled out. This might involve seeking public participation and collaboration during the very early stages of the development of any new digital health service.[49] Existing services should be monitored on usage and outcomes in different groups to understand how they are perceived and experienced by users.
When thinking about the place that digital health services have in the current UK context, it is also important to recognise that benefits from digital healthcare are heavily shaped by locality.
‘There was an app that was being trialled through the NHS to help people with sleep hygiene and stuff like that. Which I tried to sign up for but it wasn’t being run in my area, so my postcode blocked me from being able to access that service.’ – Interviewee I
‘No, no, I can’t book the appointments on the app. There is the option but my surgery have not signed up to that part of it, so if I’ll need an appointment … I’ll phone, but then that whole crisis thing, it’s half eight and be on hold for seven hours.’ – Interviewee P
‘My local housing department were absolutely fantastic, they give some families who had no access to the internet, they gave them a year’s free internet with iPads.’ – Interviewee Q
The success of digital health services for different communities may also depend on local capacity for data collection and analysis, and variation in digital skills between or even within GP surgeries too.
‘The people who do [online prescriptions processing] are not of the same calibre as the people who have been employed in reception. They don’t know the staff and so, they’re more reliant on the computer but if the computer goes wrong, as it did, you know, then people’s lives are mucked up.’ – Interviewee C
The ‘inverse care law’ describes how people who need the most healthcare are the least likely to receive it, demonstrated through GP practices in more deprived areas being relatively underfunded and understaffed compared to practices in wealthier areas.[50] Different levels of support and resource for digital transformation between regions is likely to replicate this phenomenon and perpetuate postcode lotteries, which digital health services in theory are meant to overcome.
The NHS may roll out digital health services like apps or access to online personal health records on a national level, but if a local GP or community organisation is not available or equipped to point patients towards these or help them understand how they work, then uptake may be unequal. This can exacerbate inequalities as not everyone sees the same benefits from access to new technologies.
Similarly, there is a challenge around equitable implementation of technology across the healthcare workforce, to ensure that clinicians in different groups are able to use it effectively and that it improves the quality of their work, rather than getting in the way.[51] If the resource isn’t there for staff across different regions, this could also widen the digital healthcare gap.
In the Health and Social Care Committee’s evaluation of Government commitments to digitise the NHS, policy pertaining to digital literacy of the workforce across the health and care system in England was rated ‘inadequate.’[52] It said that ‘while efforts to ensure appropriate balance between central and local responsibility for driving digitisation are welcome, we consider that the current approach of delegating responsibility for digitisation to Integrated Care Systems (ICS) without clear expectations for delivery risks maintaining or even increasing variability in digital maturity.’[53]
Implications
- Funding and incentives for addressing health inequalities should accompany commissioning, designing and development of new digital health services, with an awareness that right now inequalities are being exacerbated by not being able to get a GP or hospital appointment or call an ambulance in some areas.
- Metrics for what ‘success’ looks like for digital health services should be defined in advance to include addressing health inequalities, so that tech can be continually evaluated for its impact along these lines. This could include requiring inequalities impact assessments to be done, with marginalised groups involved in this feedback and analysis process.
- There is significant variation across regions in terms of initiatives for digital support for patients and digital skills within the workforce, which can replicate postcode lotteries in the digital context. Monitoring data would help identify gaps where more resource and training is needed, as a continuous and iterative process. Local authorities and health boards or trusts (across the UK) and ICSs (in England) could learn from each other on examples of good practice for digital inclusion and upskilling initiatives within the community.
Conclusion
In a challenging time for healthcare in the UK, where digital health services are taking centre stage and traditional care pathways are reshaped, there is a need to better understand how health inequalities intersect with technology. Without this evidence, the acceleration of digital healthcare risks widening health gaps.
For many of our participants, issues with access and the digital barrier to medical services was a key concern. Far from a ‘digital front door,’ digital routes to the health service acted more like a brick wall for many people we heard from. This could include not being able to find the right health information on an app provided by the GP, feeling like digital consultations were compromising their ability to communicate with the doctor, and coming up against ‘computer says no’ roadblocks when filling out forms online or trying to access electronic medical records.
This situation presents an opportunity to engage those with lived experience of health inequalities in the design and adoption of digital health services, and to commit to an inclusive and caring health system for the future.
Deeply held principles of patient-centred care are not at odds with digital health services or data use, but there are tensions. Flexibility, personalisation, and genuine consultation with the public will be important in the creation of successful data sharing projects and digital health services that mitigate health inequalities.
Some of the ways we see this happening include having digital health services facilitate rather than replace human relationships and enabling these services to flex to different circumstances and needs, while recognising that for some, digital isn’t the right option at all. In data sharing, work needs to be done to figure out how to use data better to improve the patient experience and make people feel heard, without compromising their privacy or over-relying on the data for personal care. Across all of this, pressures on access to care and NHS workforce must be factored in.
Summary of findings
Access to digital healthcare
In our research, we found that digital health services are making care less personal for many people experiencing socioeconomic inequalities and ongoing health concerns. Participants felt that these services were being implemented in ways that overlook or worsen structural issues like access to care. There was a widespread concern among participants around how health apps, remote care, e-consult forms, and online health advice or information platforms weren’t meeting their needs. These issues caused many of our participants to not seek the care they needed and to feel excluded from digital health services due to their age, health status, location, and socioeconomic status.
What can be done
- For commissioners, developers, designers and evaluators of these digital health services, there’s a need for to engage more closely with individuals from different backgrounds and marginalised groups to understand their experiences and design or iterate services that meet their needs.
- There were reports by some of our research participants of becoming stuck in ‘vicious circles’ on health apps and e-consult forms when seeking treatment. Developers and designers must identify the way this occurs for different patients, and provide care options that meet the needs of those who would otherwise be digitally excluded.
- Designing digital health services for use-cases that reduce friction for people who don’t have a lot of time, or who have limited technical proficiency is critical in this context. Similarly, digital health services must work for clinicians in order not to be a barrier between them and the patient.
- Local authorities can undertake digital inclusion initiatives, including providing devices, data plans, and digital literacy training to those who are digitally excluded, but need to be supported to do this by long-term funding.
- A clear finding here is that digital health services have their limits for some groups of people, and should be designed with the aim of deepening a relationship with patients and easing their interactions, not replacing those interactions with a digital interface. There should always be a non-digital option for people who need it or if things go wrong.
Health data and its uses
Data collected about people may not reflect the nuances of their lived experience, and the impact of this gap may be more significant for those with higher health burdens, or who feel less agency in the healthcare system. Our research participants had concerns around fragmentation of data, and a lack of trust in how data is shared and used by private companies. In general, participants wanted more transparency and control over how their health data is used.
What can be done
- People designing and deploying digital health services should find ways to work around limitations in quantitative or clinical data when planning healthcare interventions, by considering what important social context might be missing from datasets.
- Better understanding is needed about why some people distrust health data sharing and how that trust can be built up meaningfully – with the onus on data users and controllers like the NHS and any private partners. This might include citizen advisory groups on new data projects and demonstrating commitment to secure platforms for analysing health data.
- Issues of fragmented data compromising the patient experience could be partially addressed by improved IT systems and automation of operational and administrative tasks for clinicians.
- There is a delicate balance between improving patient experience through better data linkage and maintaining patient confidentiality: this is a live issue and one that requires further research and attention.
Seeing digital health services as part of a broader context
People we heard from in this research were acutely aware of the crisis that the NHS faces, and they felt it both in their routine interactions with the healthcare system (like booking appointments) and in perceptions of new digital health services (that they may be cost-cutting or efficiency initiatives over efforts to improve patient care).
Access to and experience of digital health services is shaped by the constraints or opportunities that exist at a local level: local capacity building for use of health data and digital connectivity is good in theory, but not if it only benefits some areas while others are left behind.
What can be done
- Those commissioning, designing and deploying digital health services must do so with a clear remit to tackle health inequalities, and an awareness that right now these are being exacerbated by the inability to see a GP or call an ambulance in some areas. Metrics for measuring the success of digital health services in tackling inequalities – for example through inequalities impact assessments – should be clear and well defined from the start of the process. Impact assessments should involve marginalised groups in feedback and analysis.
- Equitable provision of digital health services depends on clinicians’ ability to use new technology and how well supported this transition is when time and resource is tight. Digital health services that address these fundamental structural concerns and reduce admin and operational burden for clinicians may be more important now than shiny new tools that are parachuted into an under-resourced system. Health boards (across the UK) and ICSs (in England) could learn from each other on examples of good practice for digital inclusion initiatives within the community.
- To avoid ‘techno-solutionism’ in response to the challenges that the NHS faces, it is important in commissioning and development to justify why a new digital health service is the best solution to the problem that needs solving, that is, that a digital solution is not implemented just because it is new and exciting.
Next steps
The perspectives offered in this report offer an important piece of the puzzle for this complex situation and demonstrate the value of centring marginalised voices in the continuing debate.
We are keen to workshop these findings with a broader audience to identify where similarities and differences occur, and to engage with other lived experience research that explores the perspectives of a range of communities.
Methodology
To better understand people’s lived experiences of digital health inequalities in the UK, we supported six members of the public who have lived experience of poverty to become ‘peer researchers’, using participatory and peer-led participatory research methods.[54]
We provided trained the peer researchers on basic research skills and worked with them and to co-design research topics and approaches. The peer researchers then conducted interviews with a total of 26 members of their own communities about their lived experiences of and perspectives towards the increasing datafication of health and care.
We chose this peer-led and participatory approach for three primary reasons:
- To gain regionally diverse insights into how people experience digital health services in their everyday lives. By going to where people already are, we could capture experiences we don’t know about before, and therefore that we didn’t realise we’d need to understand. For example, some health inequalities are not immediately obvious if we do not root our observations in the places where people live.
- To focus on the ‘day-to-day’ of people’s lives, uncovering the more invisible and less-obvious ways that people’s health interacts with and is affected by digital health services. The lived experience of both health and digital inequality is highly contextual and is embedded in people’s everyday lives, including where they live, work, play, and access services. By observing and participating in the spaces where people actually spend time and encounter digital health services, we could gain richer insights into how different factors, including the physical environment, interact with health and digital inequalities.
- To expand the type of digital health services that would be considered, as COVID-19 retreated into the background of everyday life and people’s experiences of health and care.Digital aspects of healthcare were no longer considered ‘Covid-related changes’ but were becoming a part of business as usual.
Participatory approaches to research are most common in health sciences (public and patient involvement and engagement) and in education (Participatory Action Research), although these methods are increasingly used in other fields. Such ethnographically informed approaches are variably called PEER ethnography (Participatory Ethnographic Evaluation and Research)[55], collaborative ethnography[56] or community-based participatory research (CBPR).[57]
These approaches have some important shared aspects and key features. First, participatory approaches are not representative of the wider population, nor are they intended to be. Rather, these methods allow for deep interaction with specific groups of people and often with certain communities that share some demographic characteristic(s), such as region, socio-economic status, disability or ethnicity.
Second, these approaches are often place-based – meaning the site of research is local to the interviewer and the interviewee, which means the findings are enriched and contextualised. Thirdly, the peer researchers’ own positionality and subjectivity – that is, the fact that they have personal connections to the topics they are researching – are central to the research, and offer additional insights and knowledge that cannot be gained from the position of an outside, dispassionate and disconnected researcher.
Recruiting the peer researchers
Given our aim to investigate regional inequalities in relation to digital health services, we sought to engage with existing communities whose lived experiences would be particularly relevant. We considered possibilities of working with a range of different community groups, but it became apparent that it would be most straightforward to work with one group that had a fairly regionally diverse membership and reach.
We therefore approached the APLE Collective, a national collective of individuals who experience poverty, that work together with organisations to take positive action to eradicate poverty.[58] APLE Collective have members across the UK, who all have varied experiences of living with poverty and many of whom also have complex or ongoing health issues and complicated experiences with accessing the care they need.
Initially, 17 APLE members showed an interest in participating in the research, some as peer researchers and others as interviewees or in other roles, which we were still defining at that early stage.
In total, six of the APLE members who showed interest in the project went on to become peer researchers and remained involved in the project throughout the data collection period:[59]
- Brian, Glasgow
- Cora, Teesside
- Rosie, London
- Steven, Stoke-on-Trent
- Tracy, Stoke-on-Trent
- Caroline, Glasgow
Peer researcher field school
Through a series of ‘field school’ workshops between March 2022 and January 2023, we worked with the peer researchers to build their research skills and co-design the research materials, including a framework for ways of working, tools we would use for research, and the topics and questions for an interview guide.
The workshops followed the following structure:
| Workshop 1 – York (16 March 2022)
· Getting to know each other · Ways of working together · Introduction to data-driven systems and health · Introduction to research methods · Co-designing topics for study |
Workshop 2 – Online (5 May 2022)
· Methods training: research interviews · Methods training: notetaking and observing as research |
Workshop 3 – Guildford (10 June 2022)
· Co-designing interview guide |
| Workshop 4 – Online (22 and 25 July)
· Recapping the interview guide · Methods training: taking consent · Methods training: recording interviews and conducting reflection journals
|
Workshop 5 – Glasgow (6 Sept 2022)
· Reflections on carrying out interviews · Discussing challenges or questions · Focus-group discussion with peer researchers
|
Workshop 6 – Online (24 Jan 2023)
· Reflections on findings and analysis |
These workshops were coordinated and facilitated by researchers at the Ada Lovelace Institute, but were often added to the end of existing APLE meet-ups, so that the peer researchers were in a familiar and friendly environment. Once we had built rapport among the peer researchers, some workshops took place online to reduce the amount of travel peer researchers had to do, making it easier for them to take part.
Peer researcher-led interviews
Between August and October 2022, the peer researchers conducted interviews with members of their own communities in-person or over the phone.
When developing the interview guide collaboratively with the peer researchers, it became apparent that the distinction between ‘data-driven systems’ and ’digital health services;’ more generally might not be salient or understood by interviewees. We collectively decided that it was important to understand people’s experiences whether or not they were aware of the ‘datafied’ nature of the processes they encountered, and this paper has ended up focusing on digital health services, including but not limited to those that explicitly collect, store and analyse patient data.
Interviews lasted between 20 and 80 minutes and aimed to better understand the relationship between experiences of poverty, digital inclusion/exclusion and experiences of health and care. The interviews used a semi-structured approach and explored the following topics:
- Interviewee background and local area
- Accessing health and care services
- Understanding and perceptions of health data and medical records
- Experiences of and during the COVID-19 pandemic
The full interview schedule is included in ‘Appendix 3’.
The interviewees were recruited using a snowball method, whereby by the peer researchers invited people from their own local community – their friends, family, neighbours and colleagues – to take part in interviews. This meant that the peer researchers and interviewees had a shared understanding of local experiences, both putting the interviewees at ease when discussing sensitive or personal topics, and allowing the peer researchers to draw on their own personal and shared experiences to empathise with and enrich the findings.
Each peer researcher conducted between three and five interviews, and a total of 25 interviews took place with 26 interviewees (one was a joint interview with two participants), totalling 21 hours of interview recordings. The 26 interviewees ranged in age from 25 to 77 years old, and reflected a range of experiences with poverty, disability and/or other long-term health conditions. Table 2, below, sets out the interviewees’ demographics.
Payment
All peer researchers were paid for their time and covered for any travel costs incurred for project purposes like in-person workshops. Peer researchers were supplied with devices for recording interviews.
Limitations
As with any qualitative work, while there is richness in perspective, there are limitations around the representativeness of the peer-researchers and interviewees. Peer-researchers have intersectional experiences of marginalisation – all experiencing or having experienced poverty and all having had some long-term health concern. However, there is little ethnic diversity among the peer-researchers and the interviewees. We recognise this as a serious limitation and a gap in the data, where further research could uncover different experiences of intersecting inequalities in digital healthcare.
During the early stages of research and when co-producing the interview questionnaire at some of the field school workshops, we engaged with a more ethnically and socio-economically diverse group of peer researchers including migrants and asylum seekers. But issues with personal capacity to participate, and the timing of the project meant that potential researchers were unable to continue participation as the project went on.
This limitation reflects ongoing issues around the collection of a diverse range of experiences within health research – there are voices that remain unheard, under-represented and missing in these conversations. We recognise that this has to change for health-based outcomes to be truly community-centric.
Acknowledgements
This paper was lead-authored by Anna Studman, with substantial contributions by Andrew Strait, Mai Stafford and Mavis Machirori. Kira Allman designed the research for this paper and built the relationship with the APLE Collective; Aidan Peppin helped with interview coding and analysis.
Peer reviewers:
Dr Shoba Poduval, UCL
Zainab Garba-Sani, Stanford University
Appendix
- Interviewee demographics
| Interview# | Interviewer | Length of interview (mins) | Gender | Age | Ethnicity | Date | Region |
| 1.1 | Brian | 55 | – | – | – | – | Glasgow |
| 1.3 | Brian* | 55 | – | – | – | – | Glasgow |
| 2.1 | Caroline | 45 | F | 67 | Scottish | 27-Aug-22 | Glasgow |
| 2.2 | Caroline | 32 | F | 67 | British | 29-Aug-22 | Glasgow |
| 2.3 | Caroline | 25 | M | 34 | Scottish | 31-Aug-22 | Glasgow |
| 2.4 | Caroline | 20 | F | 65 | White Scottish | 1-Sep-22 | Glasgow |
| 3.1 | Rosie | 49 | F | 72 | White British | 23-Aug-22 | Midlands and North West |
| 3.2 | Rosie | 31 | M | 52 | Asian Pakistani | 22-Aug-22 | London |
| 3.3 | Rosie | 66 | F | 69 | White British | 22-Aug-22 | South West |
| 3.4 | Rosie | 70 | F | 77 | White British | 23-Aug-22 | South West |
| 3.5 | Rosie | 51 | M | 52 | British | 24-Aug-22 | London |
| 4.1 | Steve | 47 | M | 38 | White British | 2-Sep-22 | Midlands and North West |
| 4.2 | Steve | 49 | M | 49 | White British | 26-Aug-22 | Midlands and North West |
| 4.3 | Steve | 42 | M | 50 | British | 21-Sep-22 | Midlands and North West |
| 4.4 | Steve | 40 | M | 63 | – | 29-Sep-22 | Midlands and North West |
| 4.5 | Steve | 64 | – | 47 | White British | 29-Sep-22 | Midlands and North West |
| 5.1 | Tracy | 88 | F | 33 | White British | 5-Aug-22 | Midlands and North West |
| 5.2 | Tracy | 57 | F | 53 | White British | 3-Sep-22 | Midlands and North West |
| 5.3 | Tracy | 68 | F | 46 | White British | 12-Sep-22 | Midlands and North West |
| 5.4 | Tracy | 46 | M | 47 | White British | 29-Jun-22 | Midlands and North West |
| 5.5 | Tracy | 40 | M | 29 | White British | 30-Sep-22 | Midlands and North West |
| 6.1 | Cora | 52 | M | 25 | White British | 1-Sep-22 | North East |
| 6.2 | Cora | 52 | M | – | White British | 14-Sep-22 | North East |
| 6.3 | Cora | 28 | F | 31 | White British | 21-Sep-22 | North East |
| 6.4 | Cora | 48 | F | 50 | White British | 4-Oct-22 | North East |
*This interview was conducted with two interviewees at once.
- Interview data analysis
Recordings from the interview were transcribed into text documents and analysed by two researchers at the Ada Lovelace Institute using thematic analysis.[60] We then took the key themes and findings from this analysis back to the peer researchers in online workshops in January 2023 and May 2023, to gather their feedback, perspectives and insight to deepen and enrich the findings.
Initially, we had hoped to involve the peer researchers in the thematic analysis directly. However, doing this in a way that did not breach the confidentiality of the interview data and while ensuring all the data was processed securely and responsibly proved challenging. For this reason, we chose to first have the transcripts analysed by Ada researchers, before taking those findings to the peer researchers for further input.
While having Ada researchers do interview coding initially means that their perspectives were involved in gathering the first draft findings, we believe that this iterative and collaborative approach meant that the themes that peer researchers’ felt were salient in their interviews are still centred and emphasised in the report. It also acted as a way of member checking between Ada and the peer researchers.
- Interview guide
Interview Guide
Version: 21 July 2022
Read aloud
(feel free to adapt to the way you normally speak):
Firstly, I want to thank you for agreeing to do an interview for this research project!
The reason for this research project is to understand how data-driven systems in healthcare impact inequalities. Data is information and facts about people. Data-driven systems use computers to collect, process, and analyse data. Most of the time, we aren’t aware of data-driven systems, but they’re everywhere. Most digital platforms and technologies are data-driven.
You don’t have to know anything specific about data or digital technologies to participate in this project!
In this interview, I’ll be asking you about your experiences with healthcare in general and about things like health records, GP and hospital services and wait times, and the relationship between healthcare and other services, like benefits or mental health support.
You do not have to answer any question you do not feel comfortable with. You may ask to skip any question you do not want to answer.
But every interview is important to the project because we want to understand how you’re actually experiencing healthcare in your everyday life.
Do you have any questions before we start?
Are you happy to start?
Notes for peer researchers
Pre-interview checklist:
- Have you taken consent?
- Is your recorder on, and the timestamp moving?
- Do you have a way to take notes?
- Remember: take your time, listen with care, ask follow-up questions, and enjoy the conversation 🙂
Bold headings are themes; bullet points are suggested follow-up questions.
**Remember: you don’t have to ask EVERY question. It’s the themes of each section that are important.**
Keep it conversational, and follow the topics the interviewee wants to discuss (on the broad theme of data, digital technologies, and health).
And here are some good ways to ask for more information:
- “Could you tell me what you mean by…?”
- “Could you describe…?”
- “Could you give me an example of…?”
Interview guide
Getting to know you (part 1)
First, I’d like to ask you some questions about you and your background. This is just to get to know you a bit and to understand where you’re coming from.
KEY QUESTIONS: Please describe your local area and community to me. What’s it like?
(1) Could you please tell me a bit about where you live?
- What do you like about living in [place]? What do you not like about it?
- Are you originally from here/there? (Where did you grow up?)
- Could you describe your local area to me, what’s it like?
- Could you describe what a typical day is like for you?
(2) Could you please tell me a bit about your community? This might include people you live with, your neighbours, groups you’re part of, or your family.
- Do you have any young or elderly dependents? People you care for, or who care for you?
- Who are the people you spend the most time with? (Don’t need names or identifying information, just general descriptions.)
(3) Do you feel you know what inequalities are? Would you say you have ever experienced inequalities related to health?
- Could you please describe your experience with inequality?
- What made that an example of inequality for you?
- How do you know when things aren’t fair, or when things are unequal?
- How did that make you feel? / How does that make you feel?
Accessing services
I’d now like to ask you a bit about your experiences accessing health and health-related services.
KEY QUESTIONS: What is healthcare like in your area and what affects your access to it? What are the digital services you have to interact with?
(4) How would you describe your health?
- Do you consider yourself healthy? / Do you have any health issues that trouble you?
- Do your health needs mean you need to visit the GP often?
- Do they mean you need to spend time in hospitals or A&E?
- Do you think you have access to the care you need to live healthily? What would you change? What do you wish were different?
- What do you think of the healthcare system?
(5) Could you tell me a bit about what healthcare is available in your area?
- How would you describe access to healthcare in your local area?
- What is easy to access?
- What’s missing?
(6) What kinds of things would you say influence your access to healthcare?
- Examples might be your social circumstances, or access to information, or your family/home context – do any of these seem to affect your access to healthcare?
- What’s easy to access? (Why?)
- Hard to access? (Why?)
(7) How would you describe your access to healthcare from the pandemic to now?
- Has anything changed? How?
(8) Could you please tell me about how you typically interact with your GP service? (For example, how do you communicate/book an appointment etc.?)
- Do you use the phone/email /website…?
- When you get in touch with your GP surgery, do you feel like they get the information you give them right? (Could you explain why/why not…?)
(9) Have you had to use any apps or other digital services in order to access healthcare? Could you tell me about one?
- Could you tell me about another experience you’ve had with digital services and healthcare.
- Any other examples?
- Have you used any other apps to track or record things about your health or lifestyle, like your diet, walking, or exercise?
- Do you use any NHS apps? What’s that like?
(10) Have you received information from the NHS about apps or other digital services? Could you tell me about that information? What did you think of it?
(11) Have you ever had a health consultation by phone or by video? What was that like?
- What do you prefer? (Online vs face-to-face) Why?
(12) Thinking about your healthcare experiences, can you tell me about any times when you had to wait for services when you thought you should have been a priority?
- Why do you think you had priority/had to wait?
- What was the communication like – telling you about how long you had to wait or what the reasons were?
- What steps did you take?
Data and medical records
Now I’d like to ask you a few questions about data and medical records in particular.
KEY QUESTIONS: What do you think about how your health data is collected, used, or who it’s shared with?
(13) Could you tell me about any ways you’ve had to document your health or healthcare needs?
- How does that make you feel?
(14) What do you think of the way your medical records are kept and shared?
- What do you think about how your data is used, or who it’s being shared with?
- Do you think they’re accurate? Why/why not?
- Have you tried to correct them? Could you describe that experience for me?
- Do you ever access or see your records? (On an app, etc.)
- How do you feel about (any of) this?
(15) Have you ever felt like you haven’t understood a decision that your healthcare provider has made? Could you describe that to me? (Why was that?)
- Examples you could ask about include being put on the shielded patients list, or getting priority for certain services…
- Has your doctor/nurse/healthcare provider ever told you that they were using lots of people’s information to make decisions about your care?
(16) Could you tell me about any times you think your health or health records have been used to make other decisions in a system, like social care, or benefits…?
- Examples might include PIPs assessments, etc.
(17) Could you tell me about any times the council or other local support groups have contacted you about your health?
- Why do you think they contacted you?
- How do you think they knew to get in touch with you?
- How did that make you feel?
- Did you understand why you were being contacted? (Why/why not?)
COVID-19
Now I’d like to ask you some questions about the pandemic and how that’s affected your experience of healthcare.
KEY QUESTIONS: What do you think has changed about the healthcare systems during COVID? Could you give me some examples?
(19) Could you tell me a bit about your experience with your health and healthcare during COVID.
- Did you have to self-isolate? Shield? Could you tell me a bit about that?
- Did you understand why you had to shield or use an app? Please tell me about that.
- Did you ever use the contact tracing app? Could you tell me about that?
(20) What do you think about how technologies are being used in healthcare?
(21) Do you think anything has changed in the healthcare system since COVID? Could you tell me about that?
- Are there any other examples you can think of?
Getting to know you (part 2)
Now I’m going to ask you a couple more questions about you in general.
KEY QUESTIONS: What else would you like to tell me that I haven’t covered?
(22) Could you tell me a bit more about you…?
- Like, for instance, could you tell me about your experiences with work or employment?
- Could you tell me about any particular successes or challenges you’ve faced or are facing?
(23) What are some things you’re proud of? Or, things you find difficult?
(24) What else would you like to tell me about for this interview? (Anything I haven’t asked, you’d like to tell me about?)
Footnotes
[1] ‘Digital Transformation’ (NHS England, 2023) <https://www.england.nhs.uk/digitaltechnology/> accessed 22 August 2023.
[2] Ming Tang and Louise Greenrod, ‘Data Saves Lives – One Year On’ (NHS England, 28 June 2023) <https://www.england.nhs.uk/blog/data-saves-lives-one-year-on/> accessed 22 August 2023.
[3] ‘England Summary | Coronavirus (COVID-19) in the UK’ (GOV.UK, 17 August 2023) <https://coronavirus.data.gov.uk> accessed 22 August 2023.
[4] Ada Lovelace Institute, A knotted pipeline (2023) https://www.adalovelaceinstitute.org/report/knotted-pipeline-health-data-inequalities accessed 31 August 2023
[5] Digital exclusion describes the situation in which people and groups in society are unable to engage with digital technologies and therefore do not feel the benefits that these technologies make available to them. Reasons for digital exclusion might include financial barriers, accessibility issues, lack of requisite skills, and differing levels of motivation to use digital technologies. Honeyman, Matthew and others, ‘Digital Technology and Health Inequalities: A Scoping Review’ (Public Health Wales NHS Trust 2020).
[6] Ada Lovelace Institute, The data divide (2021) https://www.adalovelaceinstitute.org/report/the-data-divide/, accessed 22 August 2023
[7] Ben Goldacre, ‘Better, Broader, Safer: Using Health Data for Research and Analysis’ (Department of Health and Social Care) <https://www.gov.uk/government/publications/better-broader-safer-using-health-data-for-research-and-analysis> accessed 22 August 2023.
[8] Matt Whitty, ‘75 Years Young – Why Having an Innovation Culture Is so Vital to the NHS’s Longevity’ (NHS England, 1 March 2023) <https://www.england.nhs.uk/blog/75-years-young-why-having-an-innovation-culture-is-so-vital-to-the-nhss-longevity/> accessed 22 August 2023.
[9] Jonathan Benger, ‘What Does Creating a “Digital Front Door” Mean?’ (NHS Digital, 13 October 2022) <https://digital.nhs.uk/blog/transformation-blog/2022/what-does-creating-a-digital-front-door-mean> accessed 22 August 2023.
[10] ‘Digital Transformation in the NHS – Health and Social Care Committee’ (UK Parliament, 2023) <https://committees.parliament.uk/work/6694/digital-transformation-in-the-nhs/> accessed 22 August 2023.
[11] ‘Understand How Food Affects Your Body’ (ZOE, 2023) <https://joinzoe.com/> accessed 22 August 2023.
[12] ‘Predictive Wellbeing Analytics’ (MySense, 2023) <https://172.26.11.134/> accessed 22 August 2023.
[13] Ruth Lowe and Hashum Mahmood, ‘Could the Energy Crisis Cause a Public Health Emergency?’ (NHS Confederation, 19 August 2022) <https://www.nhsconfed.org/long-reads/could-energy-crisis-cause-public-health-emergency> accessed 22 August 2023.
[14] ‘The Data Poverty Lab’ (Good Things Foundation, 2021) <https://www.goodthingsfoundation.org/data-poverty-lab/> accessed 22 August 2023.
[15] Citizens Advice, ‘One Million Lose Broadband Access as Cost-of-Living Crisis Bites’ (Citizens Advice Bureau, 18 May 2023) <http://www.citizensadvice.org.uk/about-us/about-us1/media/press-releases/one-million-lose-broadband-access-as-cost-of-living-crisis-bites/> accessed 22 August 2023.
[16] ‘A Plan for Digital Health and Social Care’ (Department of Heath and Social Care and NHS England 2022) <https://www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health-and-social-care> accessed 22 August 2023.
[17] Department of Health and Social Care, NHS Digital and NHS England, ‘NHS App Hits over 30 Million Sign-Ups’ (GOV.UK, 31 December 2022) <https://www.gov.uk/government/news/nhs-app-hits-over-30-million-sign-ups> accessed 22 August 2023.
[18] Department of Health and Social Care, Steve Barclay and Chloe Smith, ‘£21 Million to Roll out Artificial Intelligence across the NHS’ (GOV.UK, 23 June 2023) <https://www.gov.uk/government/news/21-million-to-roll-out-artificial-intelligence-across-the-nhs> accessed 22 August 2023.
[19] ‘A Plan for Digital Health and Social Care’ (n 15).
[20] Ada Lovelace Institute (n 6).
[21] Ada Lovelace Institute (n 4).
[22] Khalifa Elmusharaf and others, ‘Participatory Ethnographic Evaluation and Research: Reflections on the Research Approach Used to Understand the Complexity of Maternal Health Issues in South Sudan’ (2016) 27 Qualitative Health Research 1345.
[23] Lassiter, L. E. (2005) ‘Collaborative Ethnography and Public Anthropology’, Current Anthropology, 46(1), pp. 83–106. doi: 10.1086/425658.
[24] Barbara A Israel and others, Methods for Community-Based Participatory Research for Health, 2nd Edition | Wiley (2nd edn, Wiley 2012) <https://www.wiley.com/en-us/Methods+for+Community+Based+Participatory+Research+for+Health%2C+2nd+Edition-p-9781118021866> accessed 22 August 2023.
[25] Demographic information about the peer researchers and their interviewees can be found in Appendix 1, ppxx. A limitation is that there is little ethnic diversity among the peer researchers and their interviewees, see ‘Limitations’
[26] ‘Offline and Isolated: How Digital Exclusion Impacts Access to Healthcare for People Seeking Asylum in England’ (British Red Cross 2023) <https://www.redcross.org.uk/-/media/documents/miscellaneous/british-red-cross-offline-and-isolated-report.pdf?sc_lang=en&hash=21AC9568F22D7661F69D4732B6953BE5>.
[27] Bianca Bailey Wilson and others, ‘Diverse Voices in Data’ (Understanding Patient Data 2022) <https://understandingpatientdata.org.uk/sites/default/files/2022-04/Diverse%20voices%20on%20Data%20-%20Main%20report_0.pdf>.
[28] ‘Patient and Public Involvement’ (NHS Accelerated Access Collaborative, 2021) <https://www.england.nhs.uk/aac/what-we-do/patient-and-public-involvement/> accessed 22 August 2023.
[29] Anne Alarilla, ‘What Have We Learnt from Involving and Engaging with Patients and the Public in Our Health Data Science Projects? – The Health Foundation’ (Health Foundation, 5 October 2022) <https://www.health.org.uk/news-and-comment/blogs/what-have-we-learnt-from-involving-and-engaging-with-patients-and-the-public> accessed 22 August 2023.
[30] See Glossary where we explain how we understand the difference between these two terms.
[31] Quote from a peer researcher in a research analysis workshop, January 2023.
[32] ‘A Plan for Digital Health and Social Care’ (n 15).
[33] Age can be an indicator for digital exclusion, but it’s important to note that not all older people have found digitalisation of health to be a negative thing. From the perspectives of those in our research group, it seemed that older people with experiences of intersecting inequalities around socioeconomic constraints (not owning tech or always being able to pay for data and broadband) along with ongoing health concerns (sometimes finding tech inaccessible) may be more likely to be digitally excluded.
[34] Tina Jahnel and others, ‘The Digital Rainbow: Digital Determinants of Health Inequities’ (2022) 8 Digital Health <https://journals.sagepub.com/doi/10.1177/20552076221129093> accessed 22 August 2023.
[35] Health and Social Care Committee, ‘Evaluation of Government Commitments Made on the Digitisation of the NHS’ (2023) <https://committees.parliament.uk/publications/33979/documents/186799/default/>.
[36] Pritesh Mistry and Joni Jabbal, ‘Moving from Exclusion to Inclusion in Digital Health and Care’ (The King’s Fund, 8 March 2023) <https://www.kingsfund.org.uk/publications/exclusion-inclusion-digital-health-care> accessed 22 August 2023.
[37] These could include faith-based, social or patient groups facilitated by churches or community centres.
[38] Ada Lovelace Institute (n 4).
[39] David Buck and Leo Ewbank, ‘What Is Social Prescribing?’ (The King’s Fund, 4 November 2020) <https://www.kingsfund.org.uk/publications/social-prescribing> accessed 22 August 2023.
[40] Stephanie Mulrine, Mwenza Blell and Madeleine Murtagh, ‘Beyond Trust: Amplifying Unheard Voices on Concerns about Harm Resulting from Health Data-Sharing’ (2021) 5 Medicine Access @ Point of Care 23992026211048420.
[42] Gavin Freeguard and Paul Shepley, ‘Data Sharing during Coronavirus: Lessons for Government’ (Institute for Government 2023) <https://www.instituteforgovernment.org.uk/sites/default/files/2023-02/Data%20sharing%20during%20coronavirus%20lessons%20for%20government_2.pdf>.
[43] NHS guidance on protecting patient data can be found here: ‘Protecting Patient Data’ (NHS Digital, 2023) <https://digital.nhs.uk/services/national-data-opt-out/understanding-the-national-data-opt-out/protecting-patient-data> accessed 22 August 2023.
[44] Freeguard and Shepley (n 39).
[45] Goldacre (n 6).
[46] Chris Thomas and others, ‘Healthy People, Prosperous Lives’ (IPPR 2023) <https://www.ippr.org/files/2023-04/1682577258_healthy-people-prosperous-lives-april-2023.pdf>.
[47] Sachin Ravikumar, Natalie Thomas and Sachin Ravikumar, ‘Workers Stage Largest Strike in History of Britain’s Health Service’ Reuters (6 February 2023) <https://www.reuters.com/world/uk/britain-faces-largest-ever-healthcare-strikes-pay-disputes-drag-2023-02-05/> accessed 22 August 2023.
[48] Lucie Krahulcova, ‘Techno Solutionism—Very Few Things Actually Need to Be an App.’ (Digital Rights Watch, 25 March 2021) <https://digitalrightswatch.org.au/2021/03/25/technosolutionism/> accessed 22 August 2023.
[49] Digital Scotland, ‘The Scottish Approach to Service Design’ (Scottish Government 2019) <https://www.gov.scot/binaries/content/documents/govscot/publications/advice-and-guidance/2019/04/the-scottish-approach-to-service-design/documents/the-scottish-approach-to-service-design/the-scottish-approach-to-service-design/govscot%3Adocument/Scottish%2BApproach%2Bto%2BService%2BDesign.pdf>.
[50] Rebecca Fisher and others, ‘Tackling the Inverse Care Law: Analysis of Policies to Improve General Practice in Deprived Areas since 1990’ (The Health Foundation 2022) <https://doi.org/10.37829/HF-2022-P09> accessed 22 August 2023.
[51] Tim Horton and Tom Hardie, ‘Harnessing the Potential of Automation and AI in Health Care – The Health Foundation’ (The Health Foundation, 16 February 2022) <https://www.health.org.uk/news-and-comment/blogs/harnessing-the-potential-of-automation-and-ai-in-health-care> accessed 22 August 2023.
[52] Health and Social Care Committee (n 32).
[53] ibid.
[54] For an overview of peer research methods, see: Caroline Yang and Zoe Dibbs, ‘Peer Research in the UK’ (Institute for Community Studies, the Young Foundation 2020) <https://youngfoundation.b-cdn.net/wp-content/uploads/2020/10/TheYoungFoundation-PeerResearchInTheUK-final-singles.pdf?x55643>.
[55] Elmusharaf and others (n 19).
[56] Luke Eric Lassiter, ‘Collaborative Ethnography and Public Anthropology’ (2005) 46 Current Anthropology 83.
[57] Israel and others (n 21).
[58] ‘APLE Collective’ (2023) <https://www.aplecollective.com/> accessed 22 August 2023.
[59] Peer researchers names are either their real first name, or a pseudonym as per their requests.
[60] Thematic analysis is an approach to exploring qualitative data that uses step-by-step methods to identify salient ‘themes’ within research findings. It is used to first identify commonly reoccurring codes or topics within a w dataset and then identify links or relationships between several codes to generate a ‘thematic network’. This network structures the salient themes in the dataset and can be used to describe the key findings. For more information see: Attride-Stirling, J. (2001) ‘Thematic networks: an analytic tool for qualitative research’, Qualitative research, 1(3), pp. 385–405
Related content

Access denied?
Inequalities in data-driven health systems and digital health services
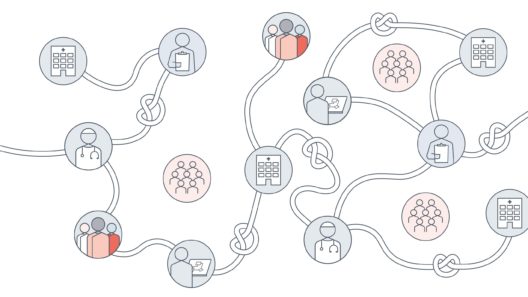
A knotted pipeline
Data-driven systems and inequalities in health and social care

The data divide
Public attitudes to tackling social and health inequalities in the COVID-19 pandemic and beyond