Access denied?
Inequalities in data-driven health systems and digital health services
18 September 2023
Reading time: 20 minutes
This briefing draws on evidence gathered from a partnership between the Ada Lovelace Institute and the Health Foundation exploring inequalities in digital health services and data-driven health systems in the UK. It sets out five challenges with accompanying recommendations for reducing inequalities and taking a more inclusive approach to digital healthcare.
It is aimed at NHS commissioners, policymakers in local and national governments, healthcare technology designers and developers, researchers, and others involved in health data and digitisation work across the private and public sectors.
This briefing is the culmination of a programme of work from 2020–23, and draws on the findings of three reports (The data divide, A knotted pipeline and Access denied?) published by the Ada Lovelace Institute.
For more information about the Ada Lovelace Institute and our work on health inequalities, contact Mavis Machirori.
Our work on health inequalities
Since 2020, the Ada Lovelace Institute and the Health Foundation have been working in partnership to explore the effect on inequalities of the accelerated adoption of data-driven health systems and digital health services during the COVID-19 pandemic, and ramifications for the future of healthcare.
The aims of this partnership were to:
- develop the evidence base around the interaction between data-driven systems and health inequalities
- build a shared understanding of actions to reduce health inequalities
- encourage prioritisation of health inequalities in the design of policy and in the development/use of data-driven systems.
This policy briefing sets out our evidence, gathered by research across four different workstreams:
- A public attitudes survey exploring access to and experience of digital health technologies.
- A landscape review of data-driven systems deployed in response to the pandemic, supplemented by the experiences of people who worked with, or drew insights from those systems.
- Participatory research gathering the perspectives on digital health services of people experiencing poverty and chronic health concerns.
- Performance analysis of a risk-prediction algorithm on different demographics.
These workstreams and relevant outputs are described in more detail at the end of this briefing.
Definitions
Data-driven health systems are made up of the people and technologies in healthcare systems that collect, process and analyse data about patients. They are not patient-facing but are used by a range of actors, including healthcare providers and data analysts, who use the information shared to deliver individual care or inform wider public health policy. Data-driven health systems are used to present health information in new ways, make predictions or reach a particular outcome. Examples include population health dashboards like the COVID-19 Data Dashboard,[1] risk-prediction algorithms and diagnostic tools.
Digital health services are patient-facing digital tools like apps or online platforms that provide health information, advice and care. These can include apps to make GP appointments, health tracking apps, online triage chatbots and portals, health advice websites and e-consult forms.
Challenges and recommendations
Our research identified several challenges in how data-driven health technologies are designed, developed and delivered, along with recommendations that address our findings.
We set these out below, alongside guiding questions to help people in different roles understand how their work can impact on inequalities.
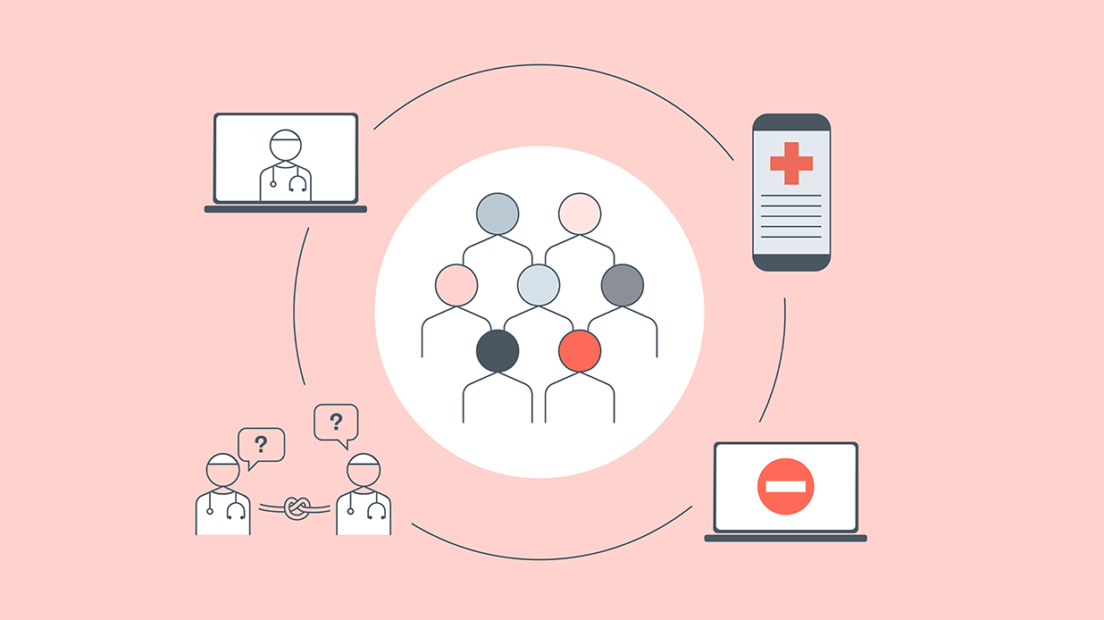
Challenge 1: Digital exclusion and access to healthcare
Digital exclusion compromises patients’ experience of or access to medical care. Digital exclusion also leads to gaps in data: if you cannot participate, your experiences are not recorded and technologies are not designed with you in mind. Digital-first or digital-only healthcare can therefore exacerbate inequalities, especially for those with complex health needs.
Recommendations
- All NHS services must provide a non-digital option for accessing healthcare to all patients Digital and non-digital options for contacting healthcare providers and having appointments should be clearly explained so patients are able to make an informed choice about which option best suits their needs.
- DHSC, devolved health departments and the NHS should fund local authorities and voluntary, community and social enterprise (VCSE) organisations to undertake digital inclusion initiatives. These should be funded on an ongoing basis rather than one-off programmes. Initiatives could include providing devices, mobile phone internet data plans and digital literacy training to those who are digitally excluded. There should be a clear framework for distributing responsibilities between local authorities, VSCEs and NHS trusts in undertaking these initiatives.
- Organisations involved in designing and developing the NHS app and other patient-facing digital health apps should embed public participation research and co-design in the development and deployment of new features. This should involve iterative, qualitative research and working with different demographic groups, particularly those that are more likely to be digitally excluded, to be less well represented in data or to experience health inequalities. This may involve – but is not limited to – citizen panels, focus groups and user research. Designers and developers should also publish clear pathways for how the input of these groups will be embedded into decision-making.
- Organisations involved in designing and developing the NHS app and other patient-facing digital health apps should collaborate with GPs and local health providers to help clinicians, patients and carers understand how to use the apps. They should also be prepared to make changes in line with feedback. Collection of feedback should be done in-person and online, and could involve drop-in sessions at community centres, and resources (both paper-based and online) distributed or advertised at GP surgeries.
Guiding questions for commissioners, developers and designers of digital health services
- What could get in the way of patients accessing this service?
- What would the effect be for a patient who wasn’t able to access or use this service?
- Who are the patients that might be digitally excluded and what are their needs?
Challenge 2: Unclear metrics for monitoring inequalities in data-driven systems
Developers and procurers of digital health services often do not establish clear metrics for what success looks like around health inequalities before a service is rolled out. Impacts are also not monitored, understood and mitigated after a service is rolled out.
Recommendations
- Commissioners and procurers of new digital health services must ensure that metrics for measuring the success of technologies 1) include tackling inequalities and 2) are established at the outset. To do this, comprehensive inequalities impact assessments for digital health services should be undertaken consistently across regions to understand how these services may exacerbate societal inequalities.
- In undertaking inequalities impact assessments, teams developing technologies must define what success looks like for new digital tools – and interrogate whether this definition aligns with the perspective of patients and frontline staff. Teams should also outline what is being done to mitigate unintended consequences from the use of technologies that could result in bias or unequitable outcomes. As a result, inequalities impact assessments may need updating – for example, by adding more targeted, specific questions that are relevant to the technology – so that they provide useful and actionable insights.
- NHS England, NHS Scotland, NHS Wales and Health and Social Care in Northern Ireland should support local NHS partners with resources and training to understand limitations and benefits in data collection and data analysis. They should provide support for public participation research so that partners have a more holistic and nuanced understanding of how digital health services are being experienced in different areas, where there is unequal uptake or where digital services are perpetuating inequalities.
- DHSC and devolved health departments should fund dedicated teams responsible for post-deployment monitoring of the impacts of digital health services on inequalities.
- DHSC, NHS England, NHS Scotland, NHS Wales and Health and Social Care in Northern Ireland should all establish guidelines for consistent inequalities impact assessments, data standards and inequalities working groups, and sharing best practice across teams.
- NHS data and digital transformation teams should include inequalities working groups that have a remit to embed inequalities impact assessments and public participation research with people experiencing health inequalities in data-sharing projects and digital health services.
- UK Research and Innovation (UKRI) and the National Institute for Health and Care Research (NIHR) should match its funding for artificial intelligence technologies in health[2] with funding for research into the impact of data-driven health systems and digital health services on inequalities.
Guiding questions for commissioners, developers and designers of digital health services
- How do new digital health services address strategic aims for reducing inequalities that have increased since the pandemic?
- How will you monitor the impacts of digital health services among different groups, and how long will this monitoring continue?
- Where could inequalities or biases arise in the lifecycle of a digital health service? How can those be mitigated?
- How have you engaged with people who might be affected by health inequalities at different stages of design, development and implementation?
Challenge 3: Lack of public confidence in data use and protection
People experiencing health inequalities don’t feel confident about how their data is being used or protected by health and care organisations and national NHS bodies. They may therefore be less inclined to participate in digital technologies, as they may not perceive that they will benefit them. They may also worry that data collected may be used for purposes they have not agreed to.
Recommendations
- NHS services should consistently communicate with the public about how their data will be used by public and private developers of data-driven health systems. This should include what modes of redress the public have if something goes wrong; which organisations digital health services are being procured from; how patients’ data will be used by these services; and what need these services are addressing – including the value for patients.
- NHS data teams should involve patients in decisions about their data. For an example of how the NHS could involve people in more direct decisions about their data, see Algorithmic Impact Assessment in healthcare (a proposal for the use of an algorithmic impact assessment for data access in an AI imaging case study, in partnership with the NHS AI Lab).[3]
- NHS, DHSC and devolved health departments should experiment with ways to involve people experiencing health inequalities in decisions about their data. This should be through expansion of the use of public participation research on new data-sharing projects. These efforts could build on initiatives like the Scottish Approach to Service Design[4] and Health Data Research UK (HDRUK)’s INSIGHT hub.[5]
- Integrated Care Boards in England, and health boards and Trusts across the UK should clarify how data is used to inform health decisions.
Guiding questions for NHS Digital Transformation, commissioners, platform developers, local government, public health partnerships and business analysts
- How will you demonstrate to the communities you serve that you are a trustworthy steward of their data?
- Have you undertaken any kind of engagement with the communities you serve to understand their views of the NHS and uses of their data?
- How can you involve members of the public in decisions about their data and how will you communicate change resulting from their feedback?
- How will you communicate with the public about decisions around their data and who has access to it?
Challenge 4: Poor data quality and lack of social context in data
At national levels, commissioners, developers, analysts and procurers of digital health services often do not have enough contextual information to understand the complexities of people’s healthcare needs. As a result they may fail to design and deploy their technologies to suit those needs.
The confluence of these two factors (poor data quality and lack of social context) exacerbates inequalities by missing individuals’ needs, or not addressing their needs in equitable ways. For example, our report The data divide shows that people earning less than £19,000 are less likely to access digital services. They are also less likely to be represented in the data collected by those services, which is then used to design future technologies. Without appropriate data linking and awareness of these contextual drivers of digital exclusion, their health needs may be deprioritised as digitisation continues.
Recommendations
- Designers and developers of new digital health services should design services with input from the communities they will impact. Engagement with service users through qualitative research, participatory research methods and user testing with a diverse group should be a required part of the development and testing process, to better understand needs that may not be represented in clinical data.
- Anyone working in data transformation should document decisions made when undertaking any change in data where information is lost or changed due to activities such as aggregation, cleaning or categorising. This allows others to identify gaps in data and how they have been accounted for, as well as where more needs to be done to address poor quality data or collect more contextual information.
- Data teams in the NHS and those developing new digital health services should adopt data standards that flag potential inequalities or biases in datasets used for health technology and AI projects, for example through the mechanisms proposed by the STANDING Together project.[6]
Guiding questions for commissioners, and developers of digital health services, and analysts and curators working with health data
- What nuance isn’t represented in the data, which might affect how people can access or use services designed with that data?
- What problems or gaps does the data show, and are there other ways to add that information in order to understand service users better?
- Are data categories standardised? How can you balance having consistent, standardised data across different NHS trusts with retaining the nuance of data gathered from frontline clinicians?
- Does the data standard match with what I know of my target community?
Challenge 5: Lack of communication across the data pipeline
Communication between different actors in the health data ecosystem is fragmented – better coordination could improve datasets and quality of insights. Working in siloes, teams may adopt processes, or procure software and platforms, that hamper system changes that would otherwise enable nuanced responses to local concerns about inequalities. For example, in the pandemic response, development and deployment of some stay-at-home measures overlooked local information, as the platforms that analysts were using did not have the flexibility to incorporate that information.
Recommendations
- Project managers and team leads should enable better communication and knowledge sharing between different roles, departments and organisations in the data pipeline (including commissioners, curators and users) to enable feedback on functionality for monitoring inequalities. There should be clear and regular lines of communication on the ways that different departments are monitoring and tackling inequalities. This would ensure better awareness of areas of overlap, which may make it possible to recognise and share points of learning.
Guiding questions for project managers and team leads in data teams
- Am I communicating with all the represented roles in the data pipeline?
- Does connecting with different roles enable new community insights to address people’s needs?
- Is there similar work happening across different departments that could enhance my work?
- How do I share knowledge of work to reduce inequalities across my team and across different departments?
Project and publications summary
Our research took place across four workstreams, resulting in four separate outputs, which are as follows:
Public attitudes survey: The data divide
We wanted to understand how different demographic groups interacted with digital health services and data-driven systems, given the rising expectation that society would adapt to life mediated by technology, especially in response to the emerging public health emergency resulting from the COVID-19 pandemic.
We commissioned a survey to measure public attitudes towards a range of technologies deployed during the pandemic (including mental- and physical-health apps, symptom-tracking apps, digital contact-tracing apps and vaccine passports).
We found that digital health services have not been experienced equally, and that there is a divide between those who have access to, and feel they have agency and control over data-driven technologies, and those who do not. This leads to a data divide – where certain groups are not represented in data and are not considered in the design and development of future healthcare technologies. The data divide is fuelled by differences in:
- access to infrastructure (like broadband, data, smartphones) and subsequently data-driven technologies
- knowledge and awareness of data-driven technologies
- use, adoption and comfort with the technologies
- reasons for using or not using the technologies.
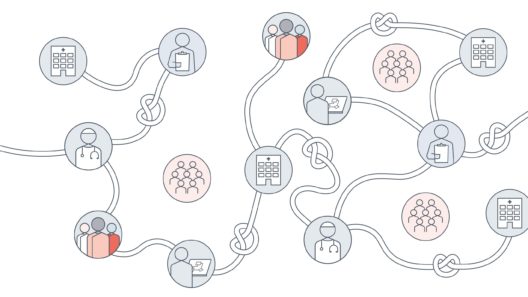
Landscape review: A knotted pipeline
We then sought to explore how some of the gaps and inequalities that emerged in the survey were thought about in the design and deployment of data-driven technologies. We conducted desk research into a range of data-driven systems used in response to the pandemic, and expert interviews with those developing, commissioning and deploying those systems.
In our resulting report we argue that the current design of the healthcare system has created a data pipeline full of ‘knots’ that disrupt the way data is transformed, from collection to analysis to system build. This has limited the ability of the health system to respond to emerging or existing inequalities in data-driven systems. Knots in the data pipeline are because of:
- minimal clarity on how to address inequalities and responsibility for doing so
- tension between local and national priorities for use of data
- poor data quality
- data curation decisions
- data being taken as a proxy for reality
- data losing its historical or social context.
Both The data divide and A knotted pipeline demonstrate that social context is not always taken into consideration in the design and deployment of data-driven systems and digital health services.
Lived experience ethnography: Access denied?
Our third workstream sought to highlight the perspectives of those with lived experience of health inequalities, collaborating with the APLE Collective, a grassroots network of individuals who experience poverty.
Access denied? used a peer research method where APLE Collective members interviewed people in their own communities about access to and attitudes towards digital services and data-driven systems in health.
Interviews found that digital health services are inflexible for those with complex health needs, which can widen health gaps, and that digital exclusion can exacerbate and fuel existing health inequalities.
There was also a feeling of frustration and powerlessness over how health data is shared and used, which made navigating and trusting healthcare services more difficult.
Taken together, these outputs summarise the ways inequalities have been impacted by existing data infrastructure and attitudes (The data divide), decisions made along the data pipeline (A knotted pipeline) and by the interaction of social context with digital tools (Access denied?).
Algorithm case study
Alongside the work done at the Ada Lovelace Institute, the Health Foundation commissioned a team from Alan Turing Institute, Public Health Scotland (PHS), National Services Scotland (NSS), the MRC Human Genetics Unit at the University of Edinburgh and Durham University to assess the performance of the SPARRA (Scottish Patients at Risk of Readmission and Admission) algorithm. Healthcare professionals use the risk score, along with their own clinical judgement and other information, to prioritise people who may benefit from anticipatory healthcare.
The case study examined whether SPARRA performed equally well across different groups based on age, sex, deprivation, ethnicity and rurality, and considered a tension between maximising overall model performance and achieving equal performance across different groups. The consequences of this tension may be of interest to patients, the public and health practitioners, who could be involved in future work on algorithmic fairness.
Acknowledgments
Workshop participants
Johan Ordish, Roche Diagnostics
Maxine Mackintosh, Genomics England, TheAlan Turing Institute
Amied Shadmaan, GE Healthcare
Andrew Davies, Association of British HealthTech Industries
Madeleine Maxwell, Homerton Healthcare NHS Foundation Trust
Shoba Poduval, University College London
Anna Dent, Promising Trouble
George Onisiforou, NHS AI Lab
Rachel Bourke, NHS Scotland
Mark Simpson, Scottish Data Board
Caitlin Ritchie, Scottish Data Board
Pritesh Mistry, The King’s Fund
Footnotes
[1] ‘England Summary | Coronavirus (COVID-19) in the UK’ (GOV.UK, 17 August 2023) <https://coronavirus.data.gov.uk> accessed 22 August 2023.
[2] ‘Artificial Intelligence Innovation to Accelerate Health Research’ (17 January 2023) <https://www.ukri.org/opportunity/artificial-intelligence-innovation-to-accelerate-health-research/> accessed 11 September 2023.
[3] Ada Lovelace Institute, Algorithmic Impact Assessment in Healthcare (2022) <https://www.adalovelaceinstitute.org/project/algorithmic-impact-assessment-healthcare/> accessed 11 September 2023.
[4] Digital Scotland, ‘The Scottish Approach to Service Design’ (Scottish Government 2019) <https://www.gov.scot/binaries/content/documents/govscot/publications/advice-and-guidance/2019/04/the-scottish-approach-to-service-design/documents/the-scottish-approach-to-service-design/the-scottish-approach-to-service-design/govscot%3Adocument/Scottish%2BApproach%2Bto%2BService%2BDesign.pdf>.
[5] Jack Hardinges and Tara Lee, ‘INSIGHT: Exploring Access to Eye Health Data’ (The ODI) <https://www.theodi.org/project/insight/> accessed 11 September 2023.
[6] ‘Draft Recommendations for Healthcare Dataset Standards Supporting Diversity, Inclusivity, and Generalisability.’ (STANDING Together 2023) <https://drive.google.com/file/d/1ZNjlrwKzyizDHFCezLHAxZm3jNchbtPm/view?usp=sharing&usp=embed_facebook> accessed 11 September 2023.
Related content

Access denied?
Socioeconomic inequalities in digital health services
A knotted pipeline
Data-driven systems and inequalities in health and social care

The data divide
Public attitudes to tackling social and health inequalities in the COVID-19 pandemic and beyond